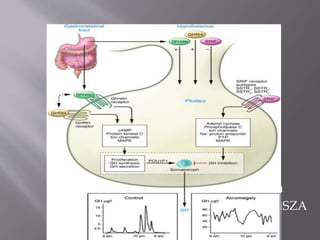
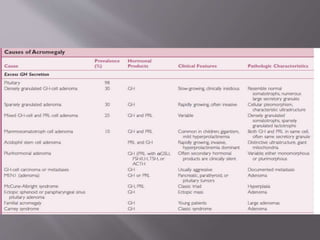
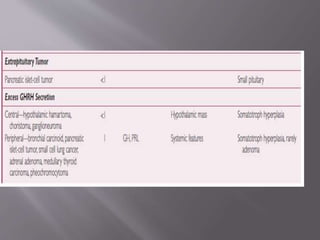
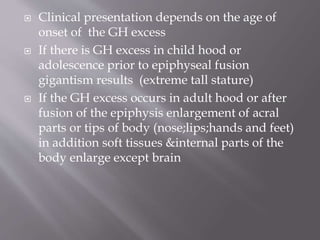
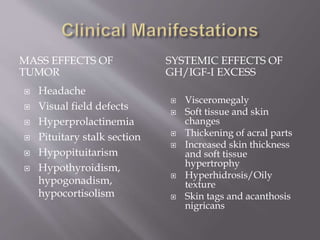
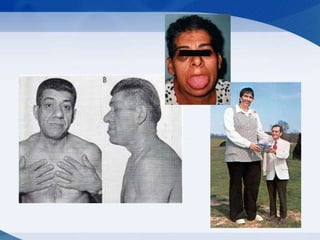
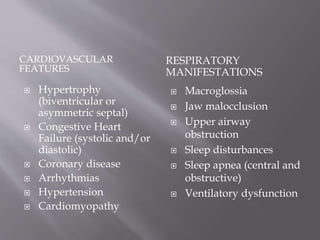
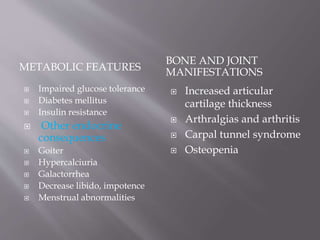
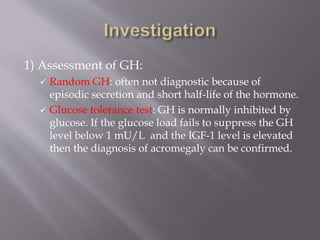
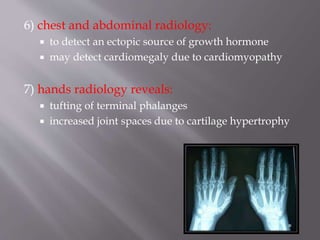
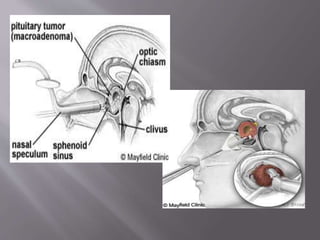
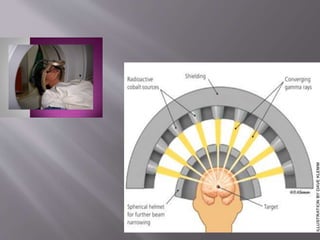
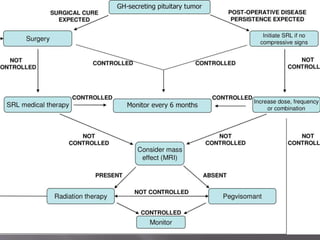
This document discusses acromegaly, a condition caused by excessive growth hormone production leading to disproportionate skeletal and soft tissue growth. It begins by describing the causes and effects of excess growth hormone, then discusses clinical features of acromegaly including organ enlargement and metabolic complications. The document outlines diagnostic tests for acromegaly focusing on growth hormone and IGF-1 levels. Treatment aims to control growth hormone levels and includes surgery, radiation therapy, somatostatin analogues, dopamine agonists, and growth hormone antagonists.