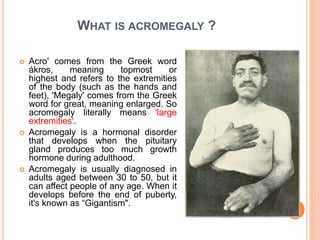
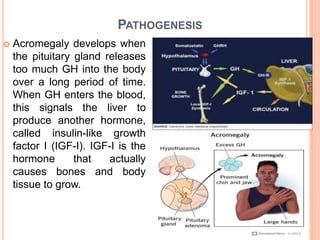
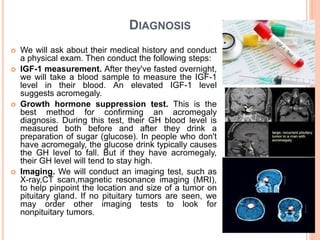
Acromegaly is a hormonal disorder resulting from excessive growth hormone production by the pituitary gland, leading to enlarged extremities and other symptoms, often caused by pituitary adenomas. Diagnosis typically involves measuring insulin-like growth factor 1 (IGF-1) levels and conducting imaging tests, while treatment options include surgery, medications, and radiation therapy to control hormone levels and tumor size. A case study discusses a 35-year-old woman treated with transsphenoidal surgery, resulting in significant health improvements.






![REFERENCES
[1] Lavrentaki A, Paluzzi A, Wass JA, Karavitaki N. Epidemiology of acromegaly:
review of population studies. Pituitary. 2017;20(1):4–9.
[2] Chanson P, Salenave S, Kamenicky P. Acromegaly. In: Fliers E, Korbonits M,
Romijn JA, eds. Handbook of clinical neurology. Vol 124. 1st ed. Waltham, MA:
Elsevier B.V.; 2014:197–219.
[3] Katznelson L, Laws ER Jr, Melmed S, et al. Acromegaly: an endocrine society
clinical practice guideline. Journal of Clinical Endocrinology and Metabolism.
2014;99(11):3933–3951.
[4] Paragliola RM, Salvatori R. Novel somatostatin receptor ligands therapies for
acromegaly. Frontiers in Endocrinology. 2018;9:78.](https://image.slidesharecdn.com/acromegaly-230725073028-579afc41/85/Acromegaly-pptx-20-320.jpg)
