- This document discusses various respiratory illnesses and lung diseases, including their symptoms, causes, diagnosis, and treatment.
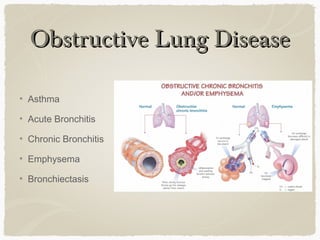
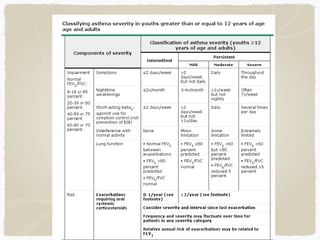
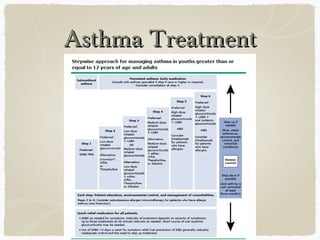
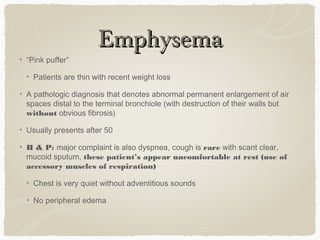
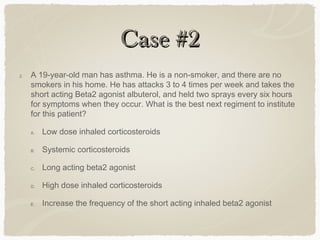
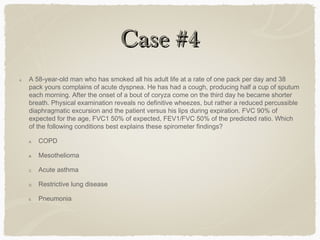
- Common respiratory illnesses covered include asthma, acute bronchitis, COPD (chronic bronchitis, emphysema), bronchiectasis, and various respiratory infections like pneumonia.
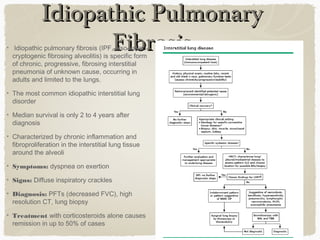
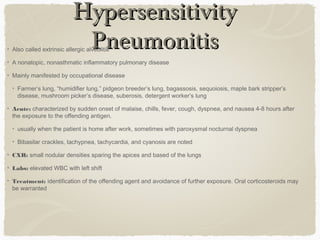
- Restrictive lung diseases discussed are idiopathic pulmonary fibrosis, hypersensitivity pneumonitis, and pulmonary eosinophilia.
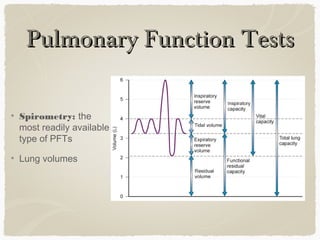
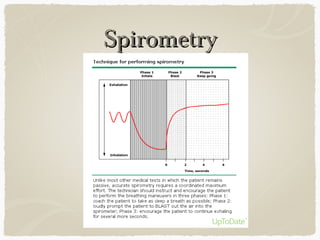
- Tests like spirometry, lung volumes, and arterial blood gases are used to diagnose and characterize respiratory conditions.