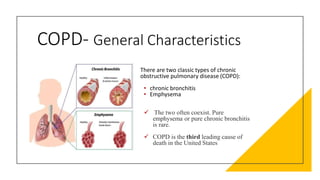
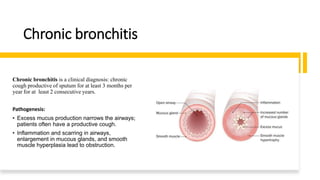
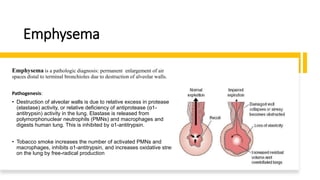
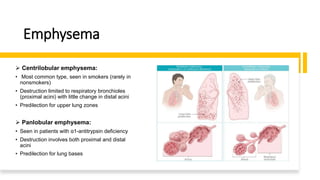
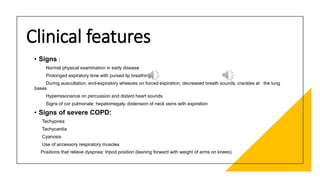
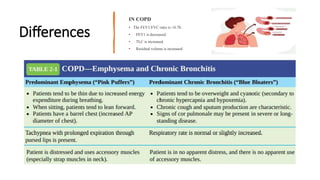
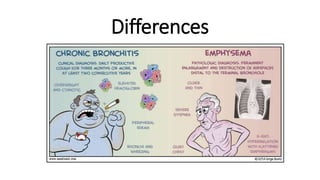
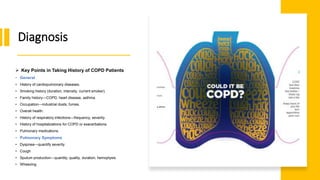
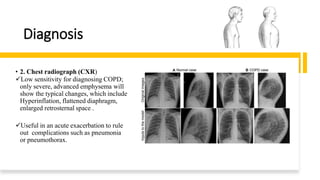
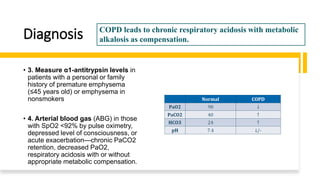
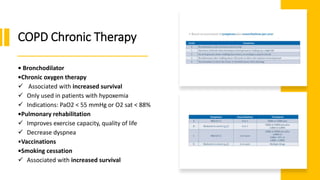
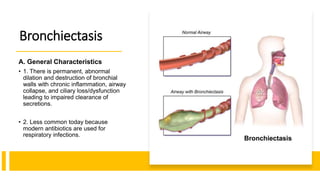
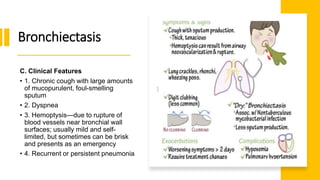
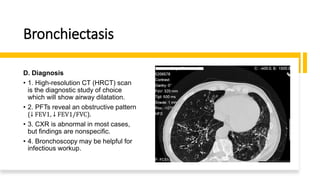
The document outlines obstructive lung diseases including COPD and bronchiectasis, describing their general characteristics, causes, clinical features, diagnosis, and treatment. COPD is discussed in detail including risk factors like smoking, clinical manifestations of chronic bronchitis and emphysema, diagnostic testing with PFTs and CXR, and treatment focusing on bronchodilators, oxygen therapy, and rehabilitation. Bronchiectasis is also summarized covering causes like infection and cystic fibrosis, symptoms of cough and sputum, diagnosis via CT or PFTs, and treatment centered around airway clearance and antibiotics.