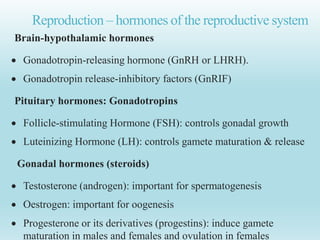
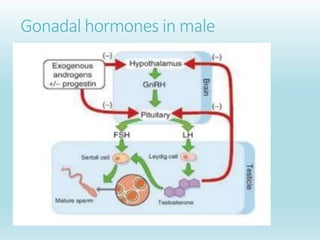
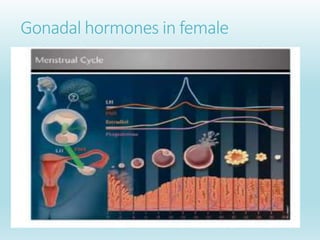
The gonads are the organs that produce gametes. In males the gonads are the testes and in females they are the ovaries. The gonads produce hormones that regulate the reproductive system. Gonadotropin-releasing hormone stimulates the pituitary gland to release follicle-stimulating hormone and luteinizing hormone, which act on the gonads. The testes produce testosterone under the influence of LH and the ovaries produce estrogens and progesterone under the influence of FSH and LH. These hormones regulate gamete production and maturation in the gonads as well as secondary sex characteristics.