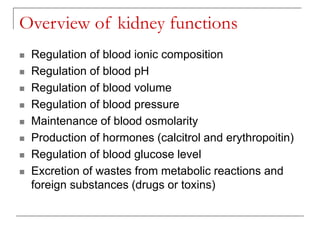
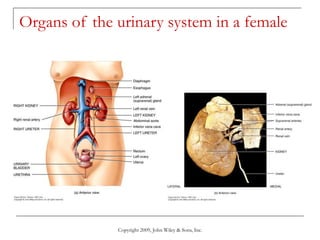
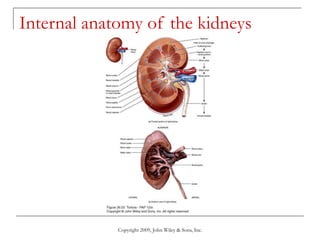
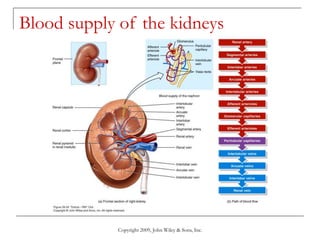
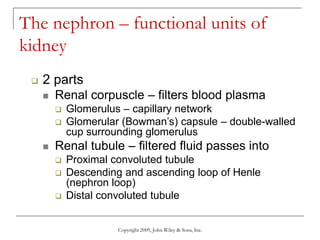
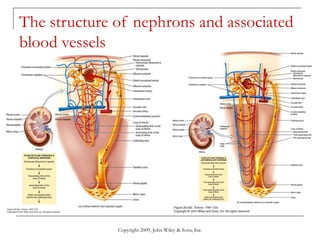
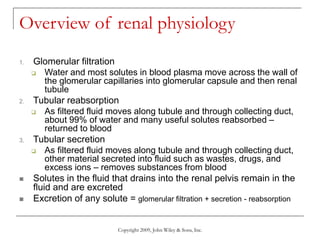
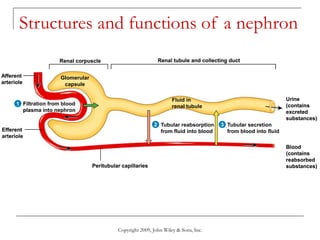
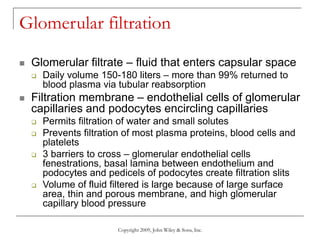
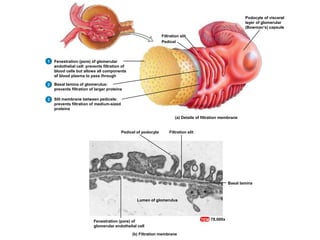
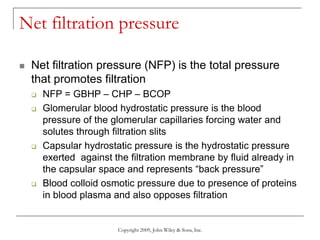
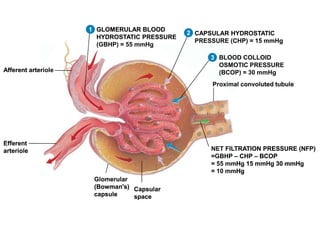
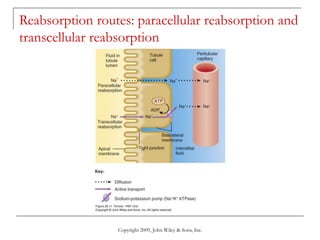
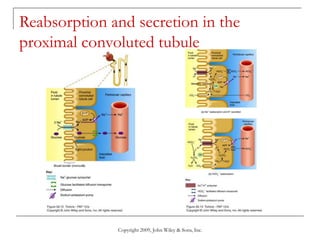
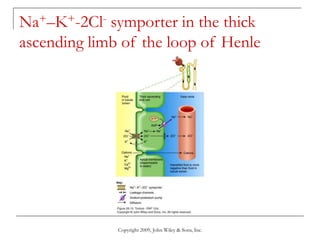
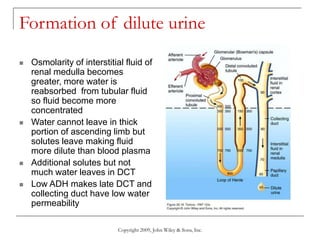
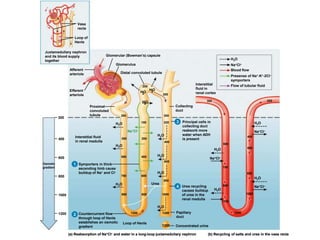
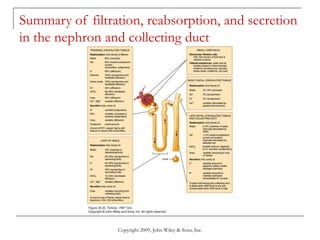
The document provides detailed information about the anatomy and physiology of the urinary system. It describes the key functions of the kidneys, which include regulating fluid and electrolyte balance, blood pressure, and blood pH. The basic unit of the kidneys is the nephron, which filters blood to form urine and reabsorbs necessary substances like water and electrolytes. Glomerular filtration occurs through specialized blood vessels that allow filtration based on size. Tubular reabsorption and secretion then modify the filtrate as it passes through the nephron before being excreted as urine.