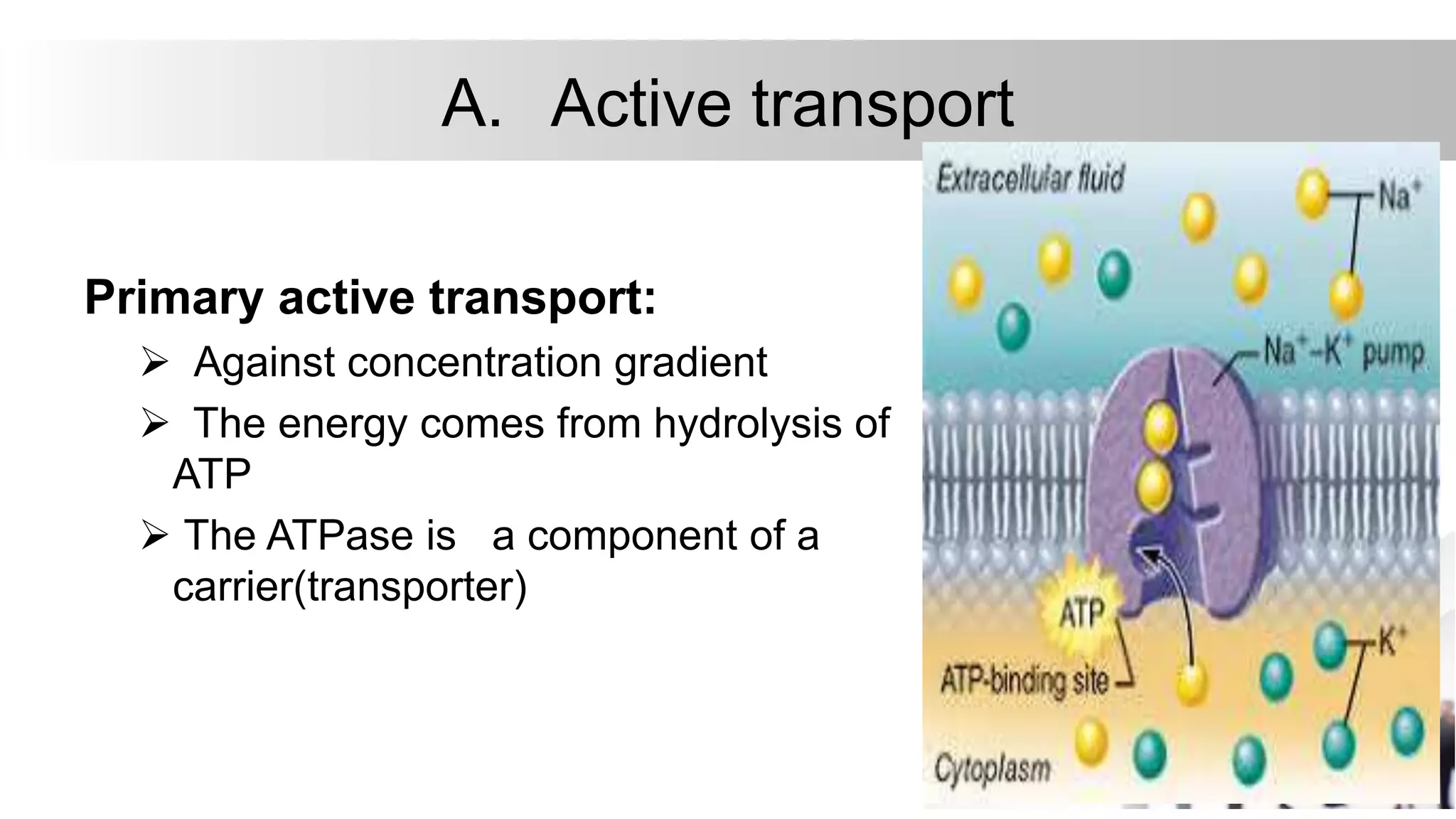
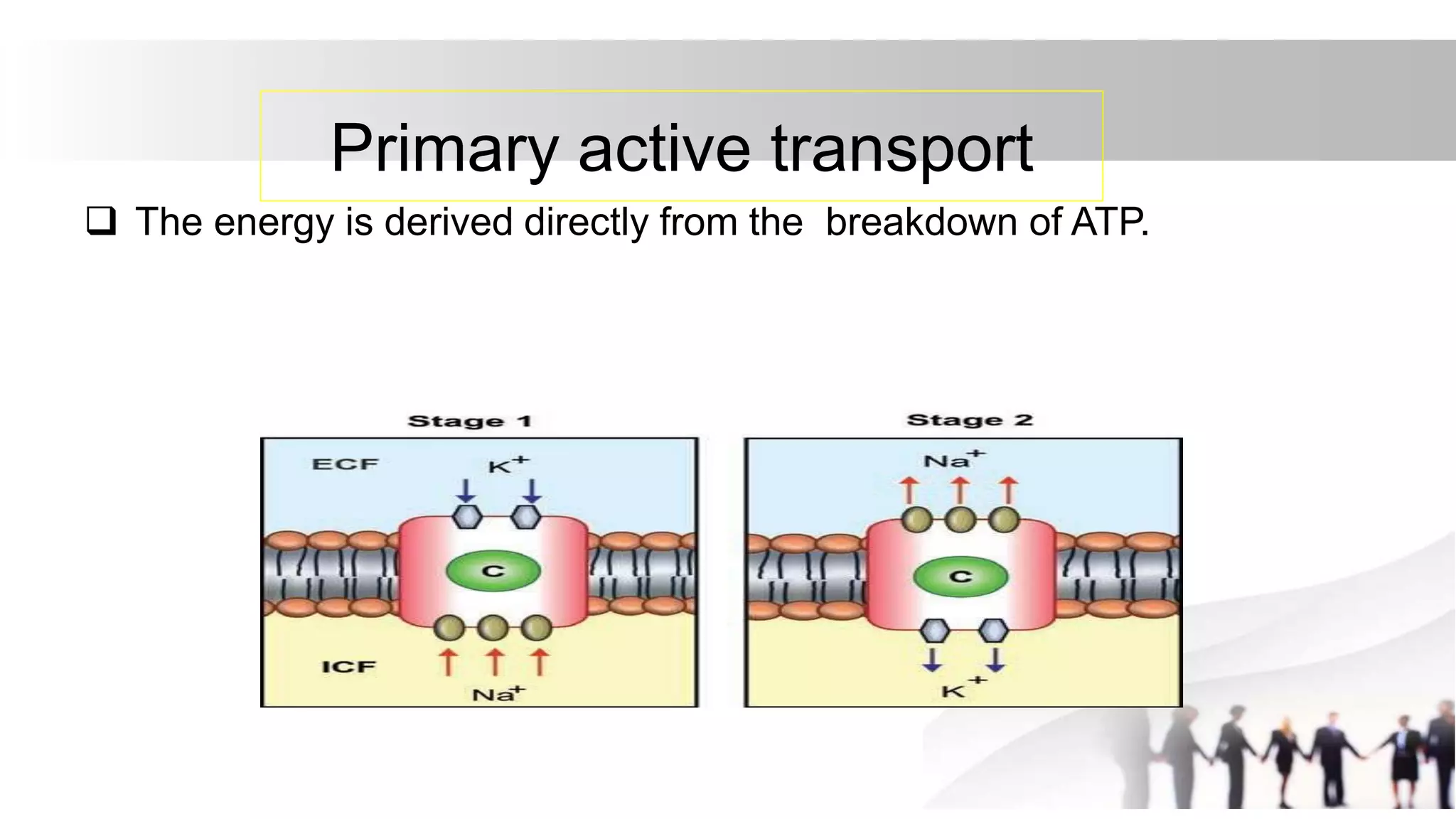
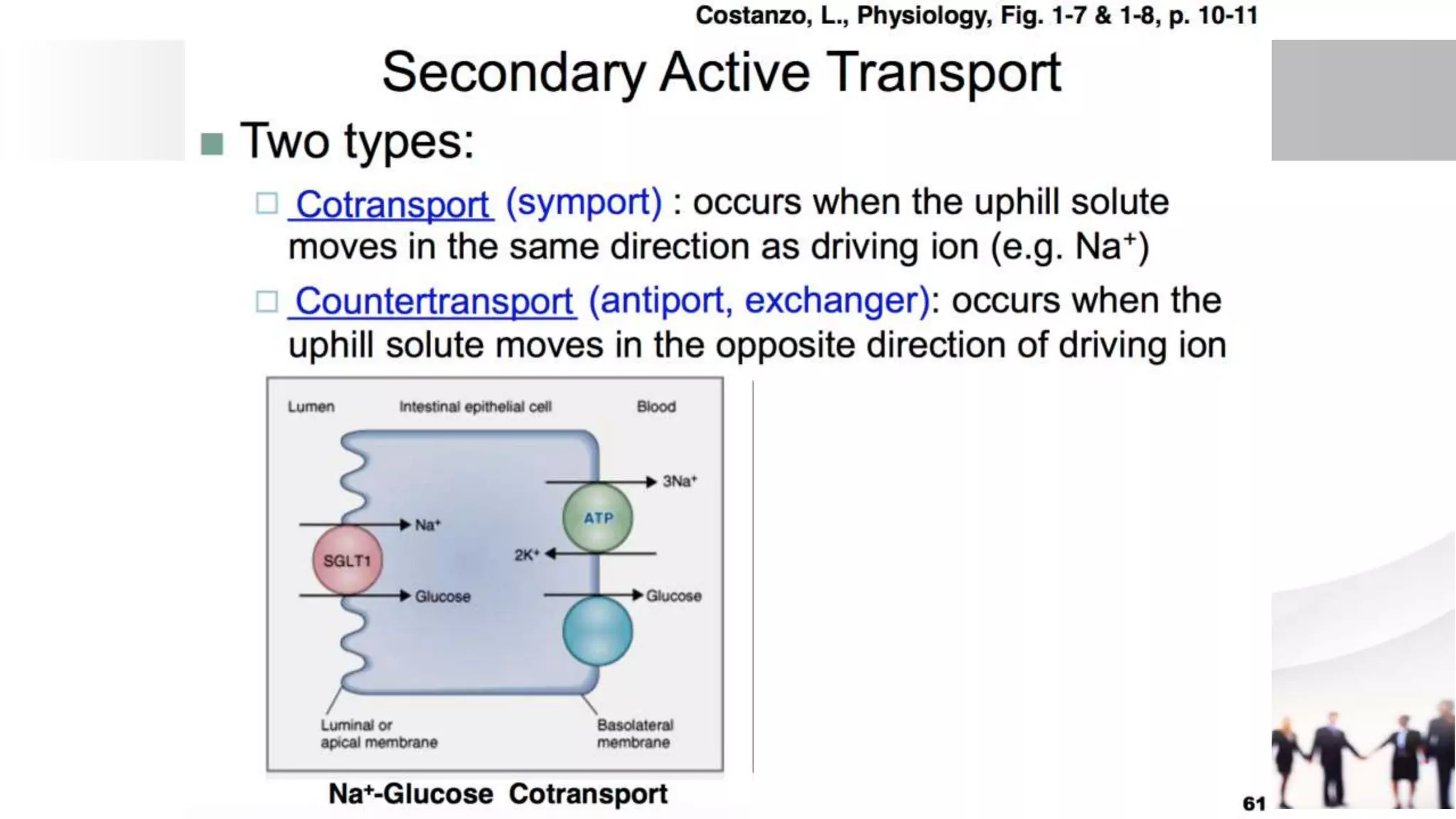
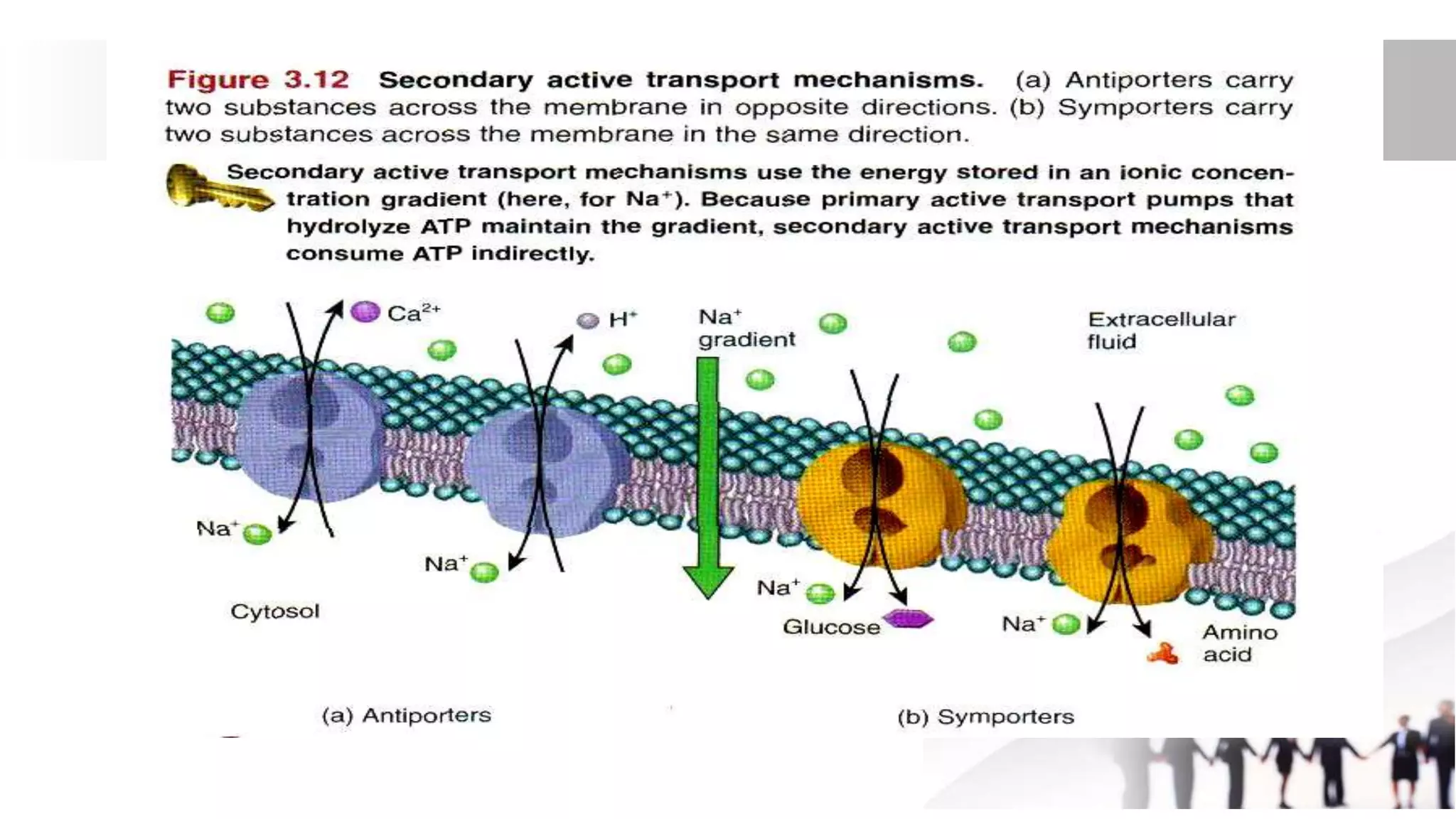
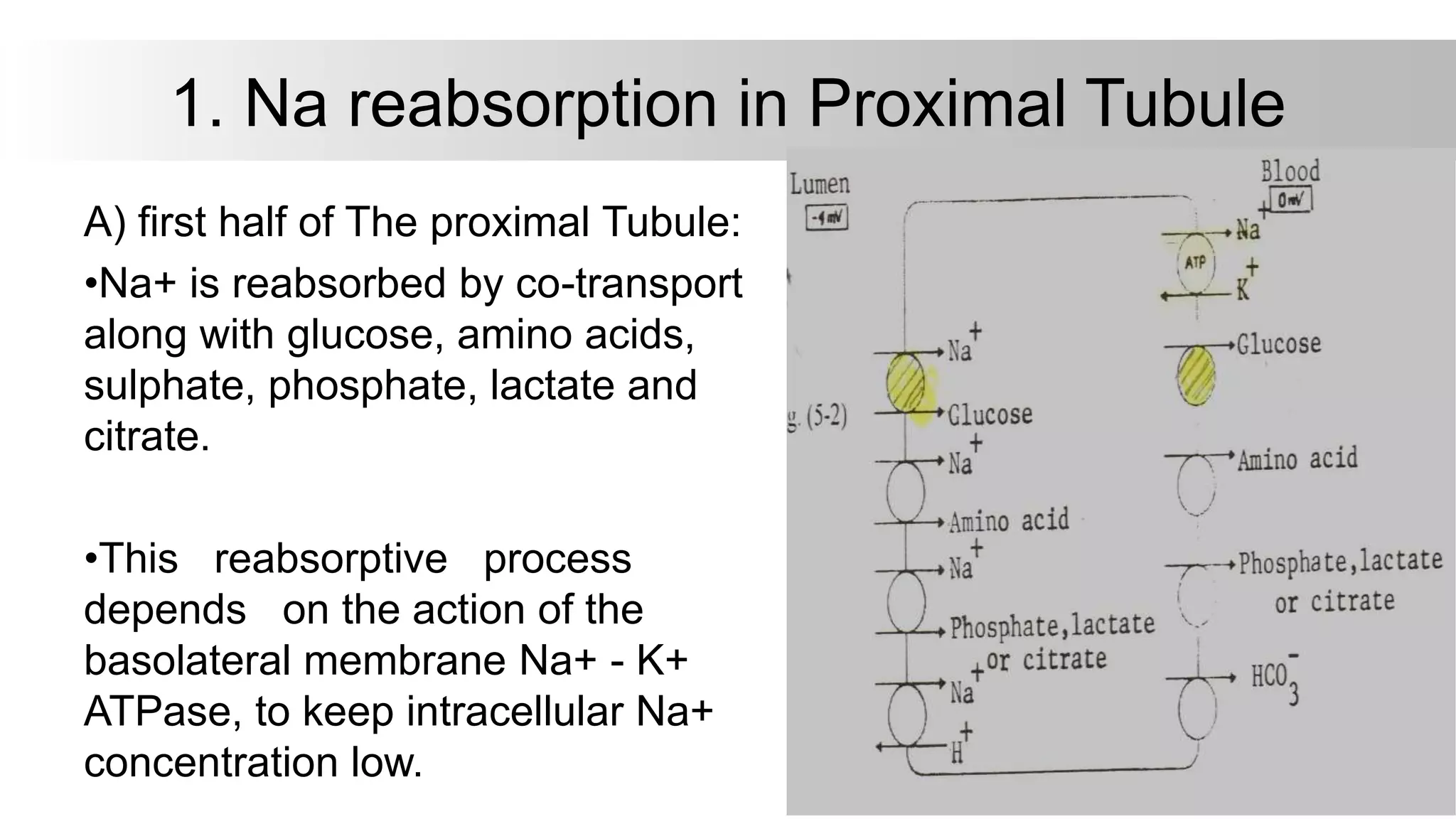
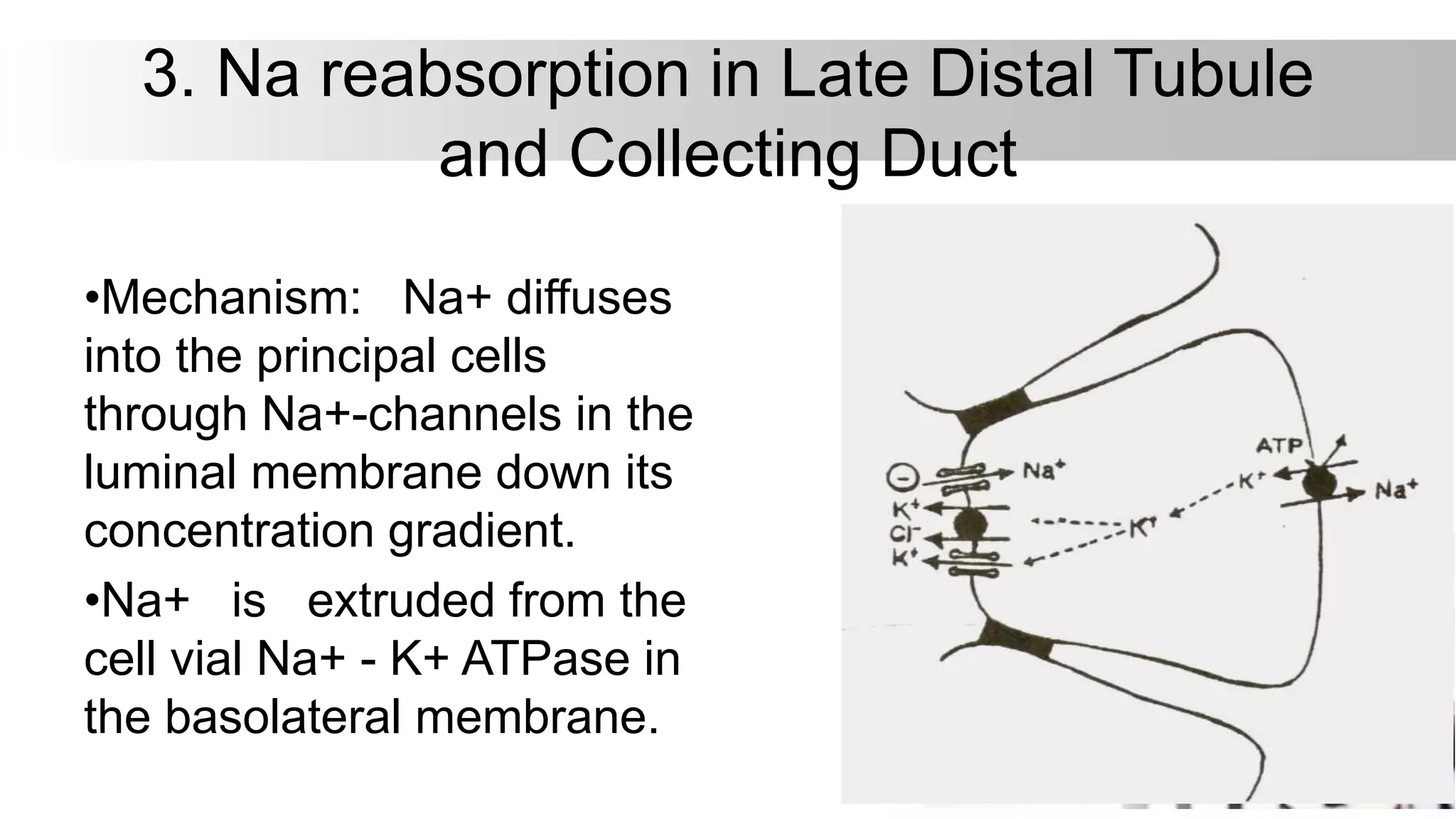
This document discusses renal physiology with a focus on tubular transport mechanisms. It describes the different types of transport including primary and secondary active transport, as well as passive transport and pinocytosis. Primary active transport directly uses ATP to transport solutes against concentration gradients using carrier proteins like sodium-potassium ATPase. Secondary active transport couples transport of one solute to the gradient of another, like sodium-glucose co-transport. The document then discusses sodium handling by the renal tubule and factors regulating sodium excretion like GFR, tubular flow rate, hormones, and diuretics. Finally, it covers glucose transport via sodium-glucose co-transport in the proximal tubule and concepts of tubular transport maximum and renal