"This comprehensive PowerPoint presentation provides a detailed overview of the physiology of the endocrine system. Explore the intricate network of glands, hormones, and their target tissues that regulate essential bodily functions. Learn about the mechanisms of hormone action, including receptor binding and signal transduction. Discover the roles of major endocrine glands like the pituitary, thyroid, adrenal, and pancreas in maintaining homeostasis. This presentation is ideal for students, educators, and healthcare professionals seeking a clear and concise understanding of endocrine physiology. Key topics covered include:
* Hormone classification and synthesis
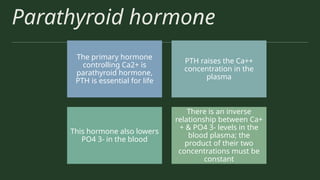
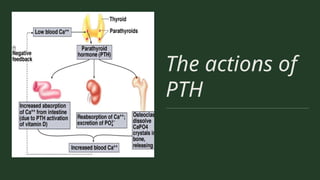
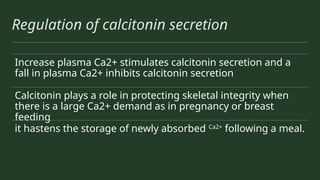
* Feedback mechanisms and regulation
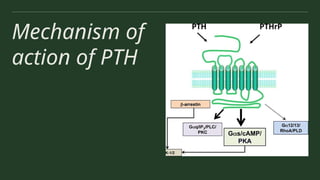
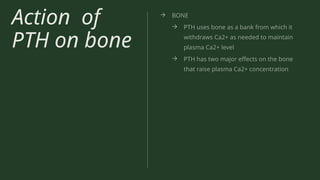
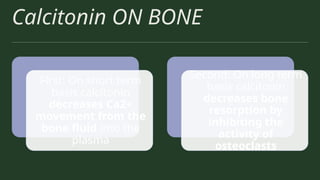
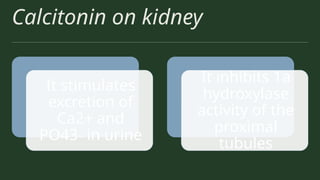
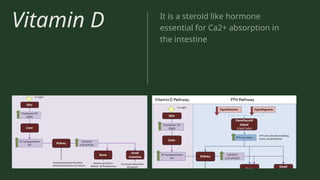
* Specific gland functions and associated hormones
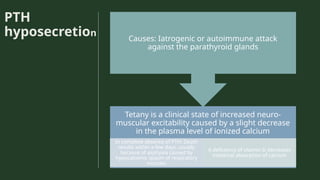
* Common endocrine disorders and their physiological basis
* Clinical correlations and applications
Whether you're preparing for an exam, teaching a class, or simply interested in the fascinating world of endocrinology, this PowerPoint offers a valuable resource for mastering the core principles of endocrine physiology."