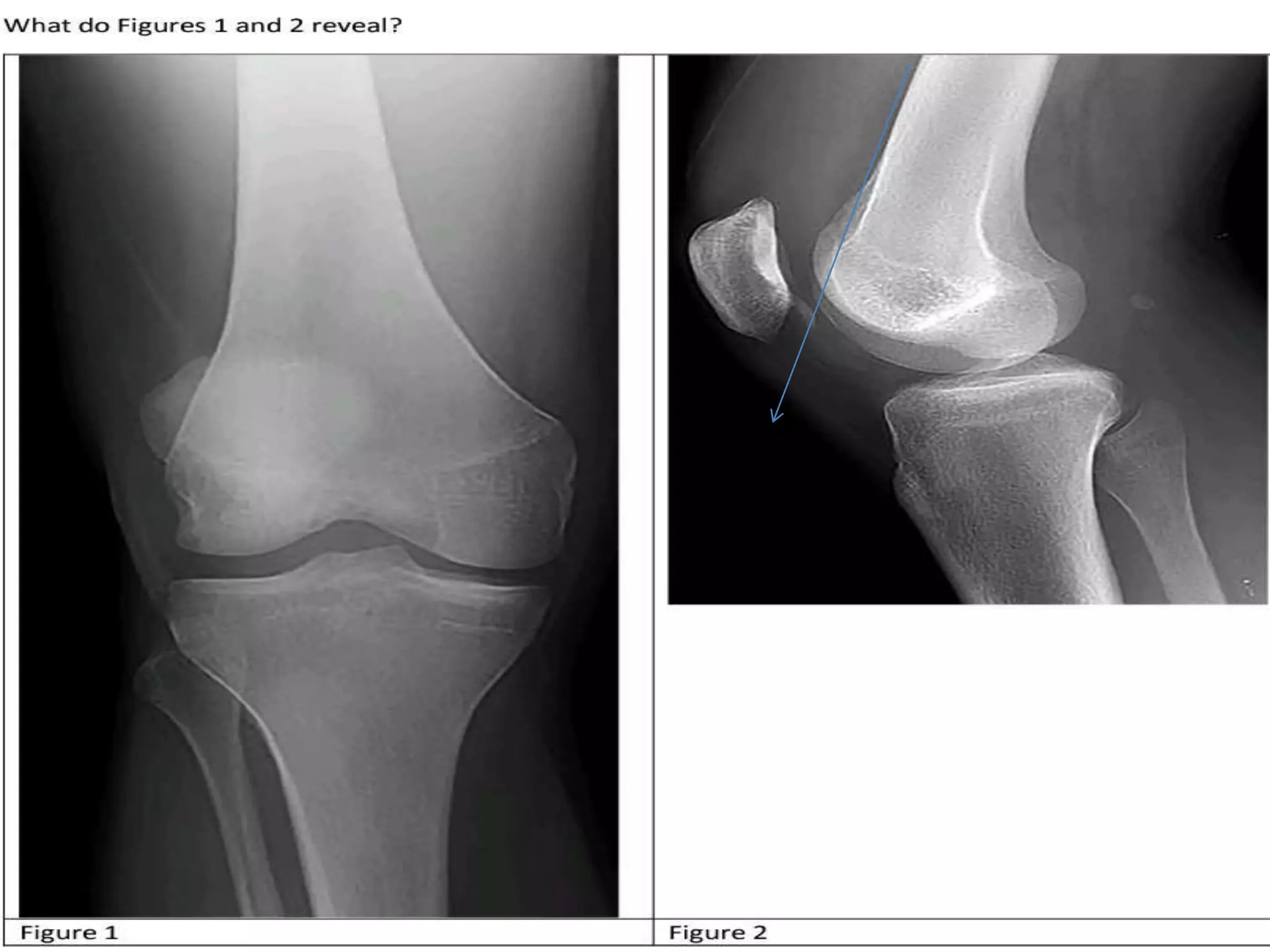
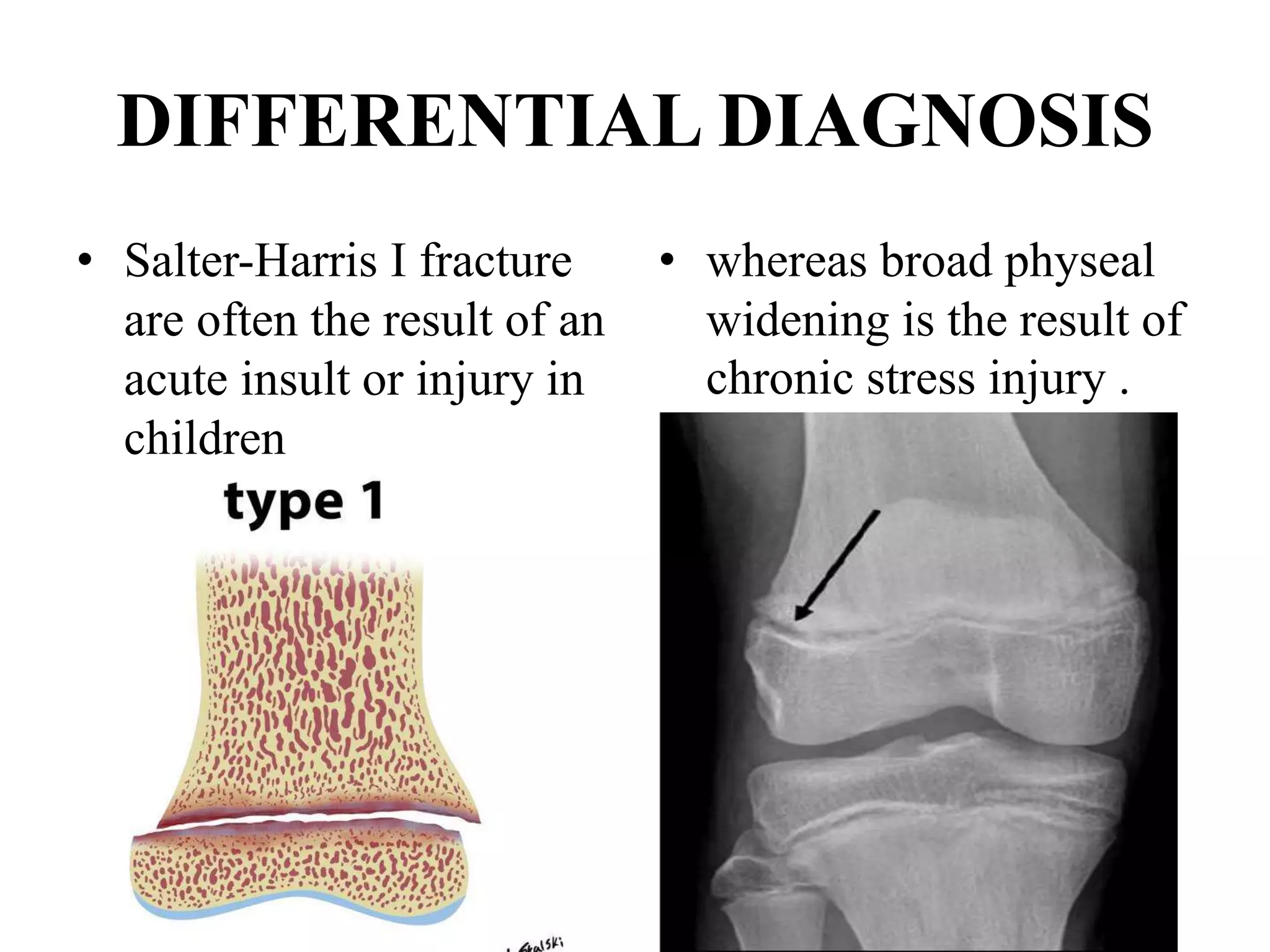
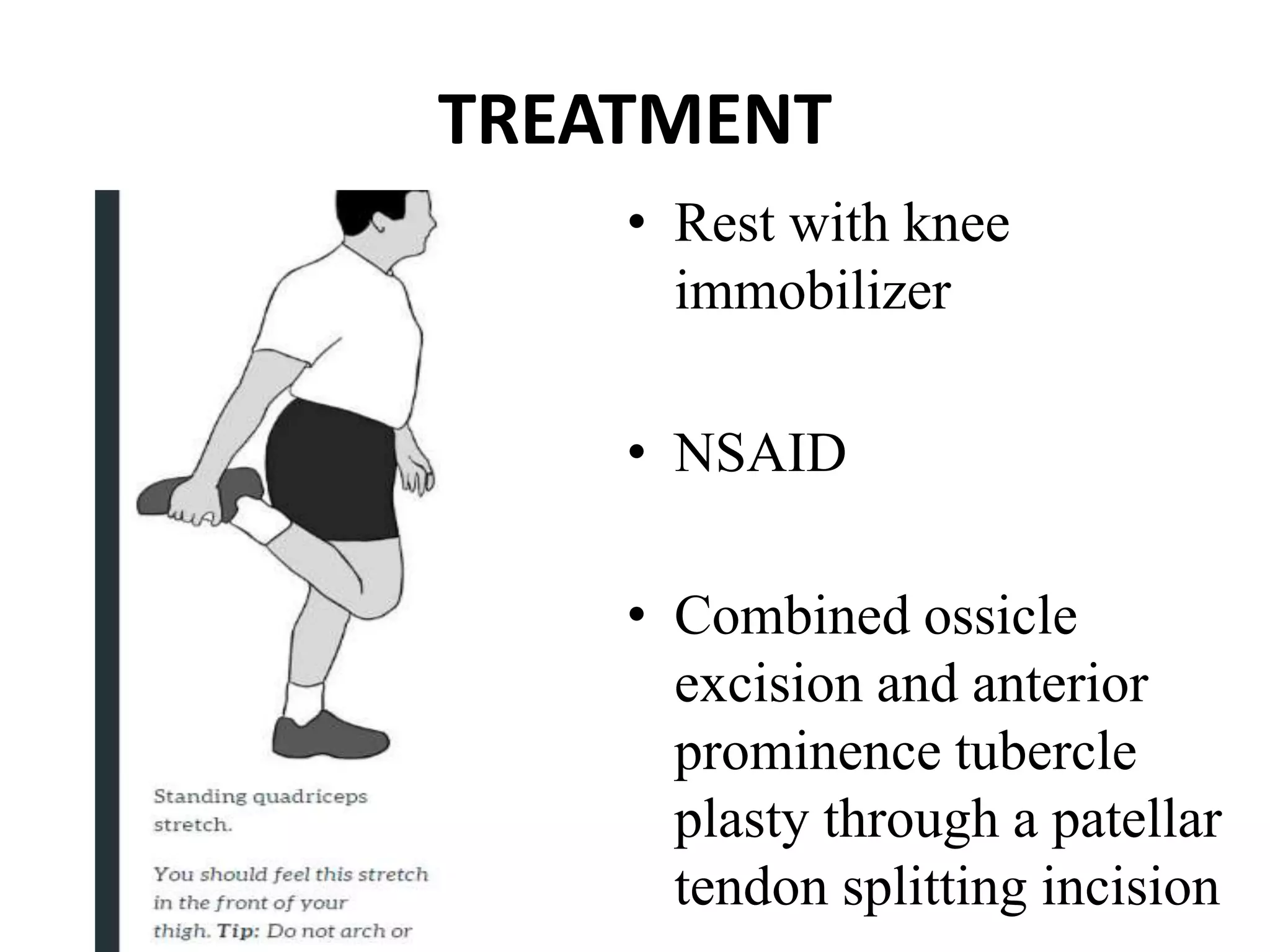
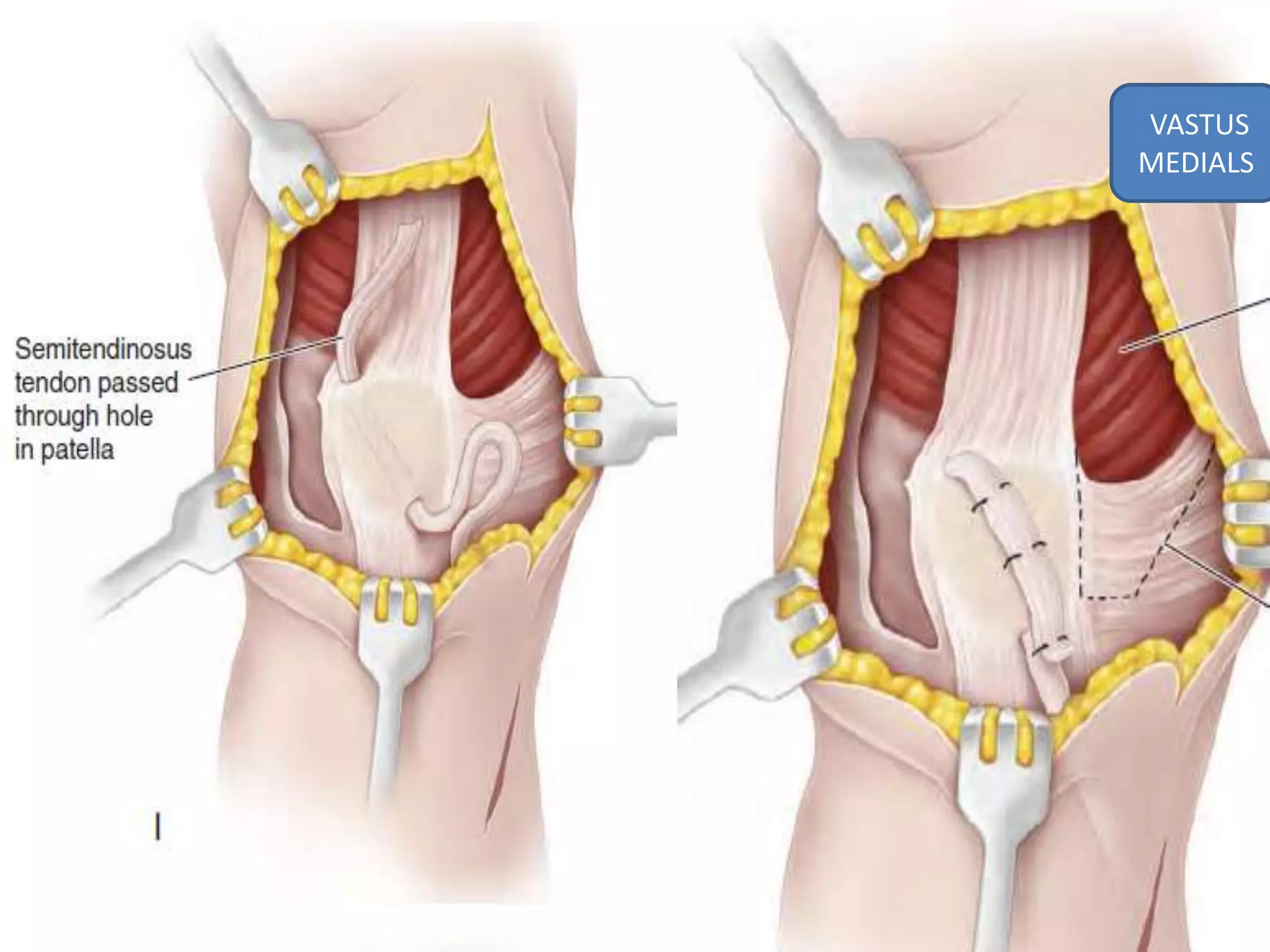
A 16-year-old boy presented with recurrent patellar dislocations while playing soccer. On examination, he had tenderness around the patella, decreased range of motion, and a positive patellar apprehension test. An MRI showed widening of the medial femoral condyle physis, consistent with a chronic stress injury from repetitive trauma. Treatment options included bracing, physical therapy, and protected weight bearing to allow healing of the physis. Surgical options like tibial tubercle anteromedialization or MPFL reconstruction were not required given the MRI findings suggested a chronic injury rather than an acute tear or malalignment.