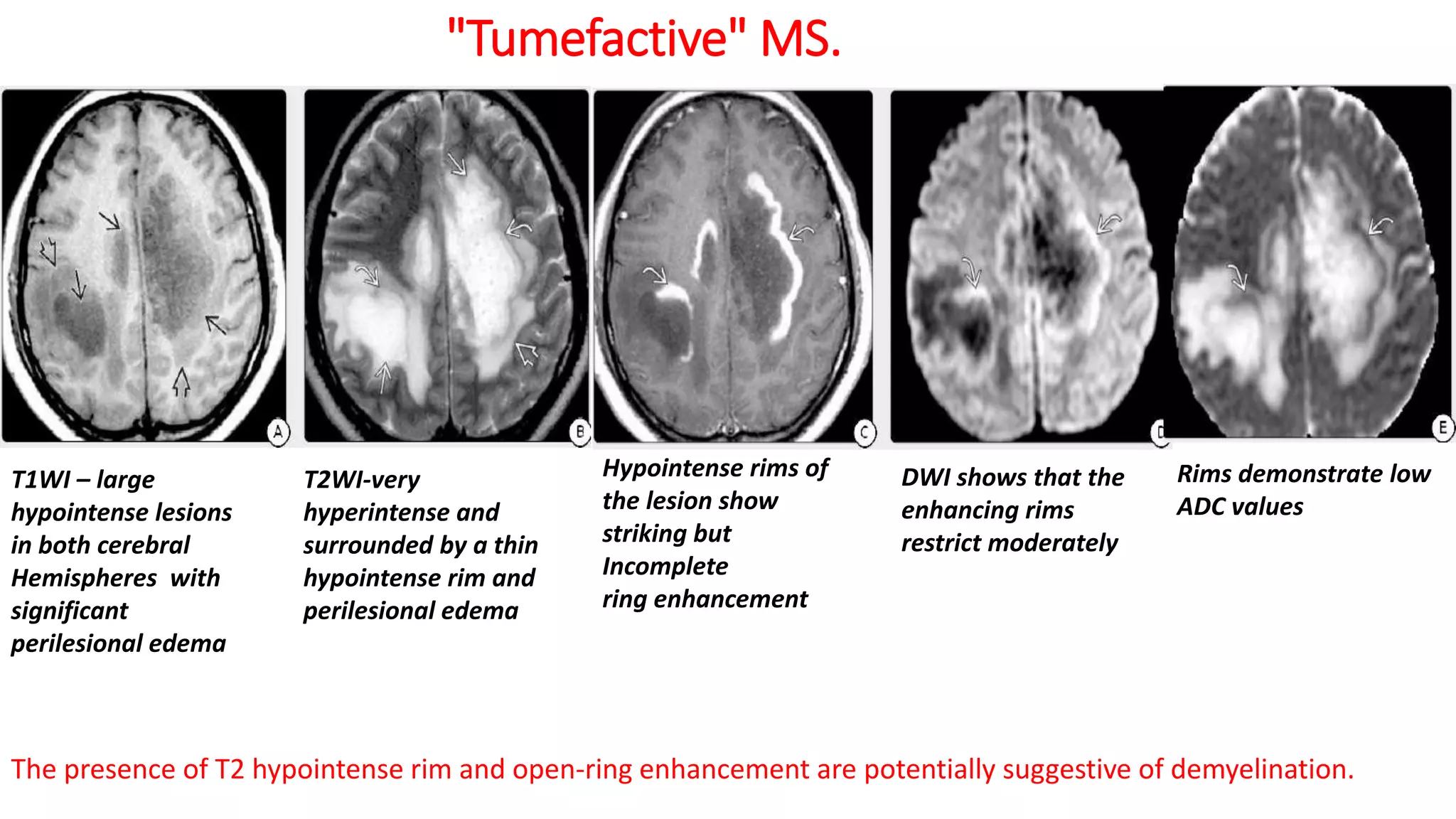
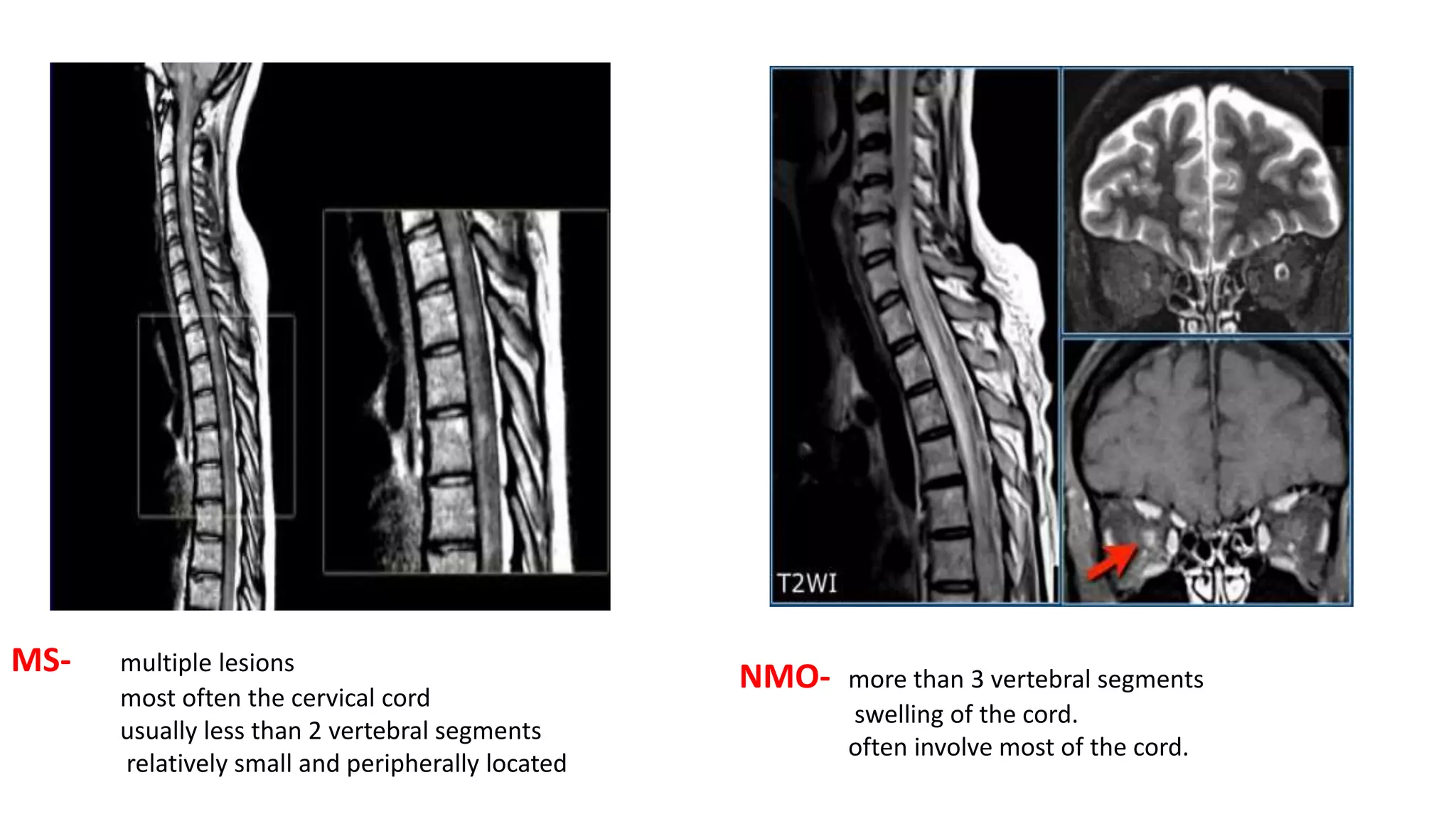
This document discusses various demyelinating diseases that can be imaged in neurology. It provides images and descriptions of findings for multiple sclerosis, ADEM, NMO spectrum disorder, Susac syndrome, CLIPPERS, acute disseminated encephalomyelitis, acute hemorrhagic leukoencephalitis, acute necrotizing encephalopathy, and osmotic demyelination syndrome. It compares imaging features of MS and NMOSD that can help differentiate the two conditions. The document also discusses variants of MS like Marburg disease, Schilder disease, and Balo concentric sclerosis.