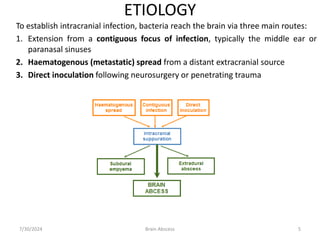
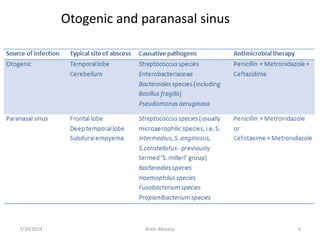
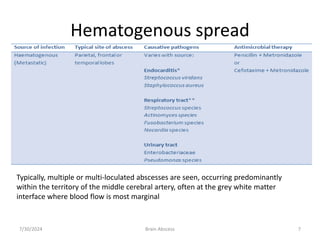
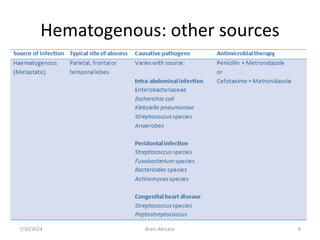
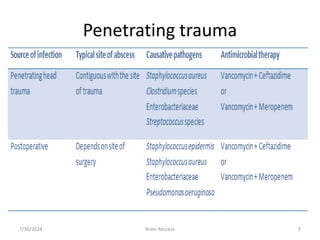
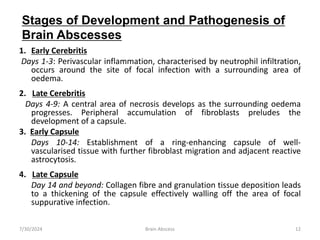
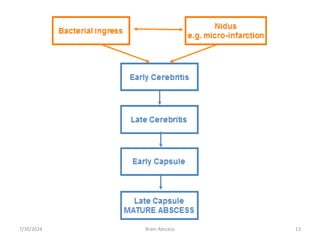
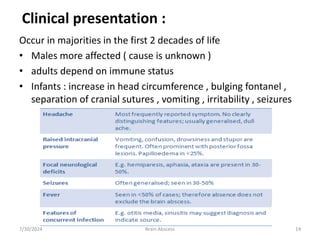
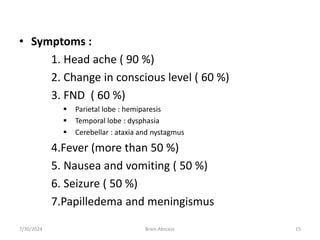
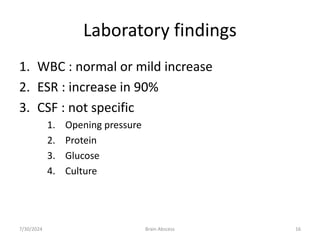
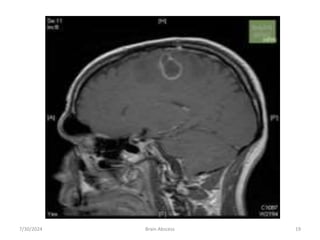
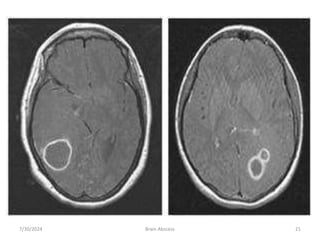
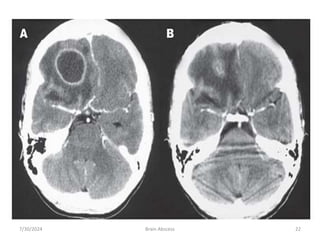
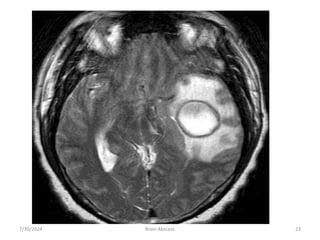
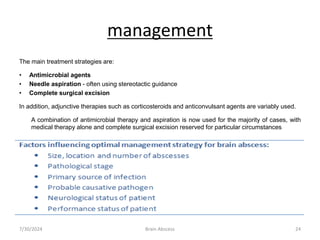
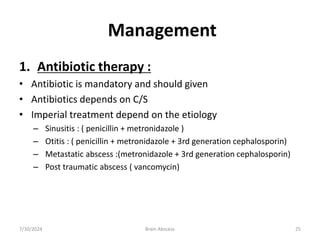
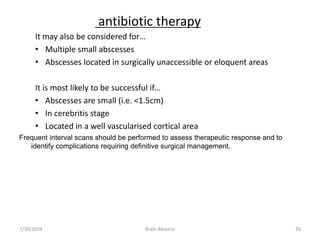
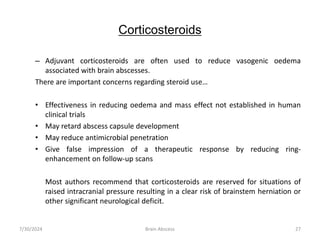
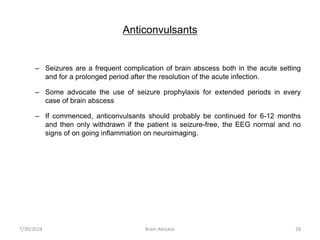
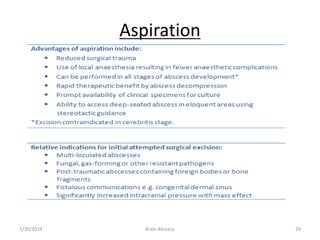
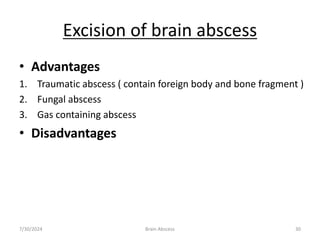
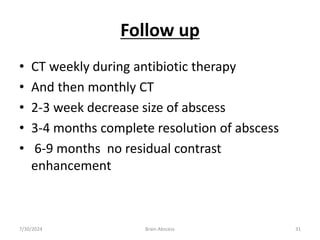
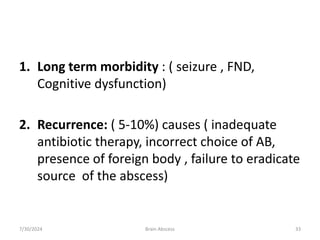
The document provides an overview of brain abscesses, covering their incidence, etiology, pathogenesis, clinical presentation, diagnosis, and management strategies. It highlights the typical pathogens involved, outlines stages of development, and discusses treatment options including antimicrobial agents and surgical interventions. Moreover, it presents information on related complications such as subdural and epidural empyema, emphasizing the importance of proper diagnosis and tailored management for successful outcomes.