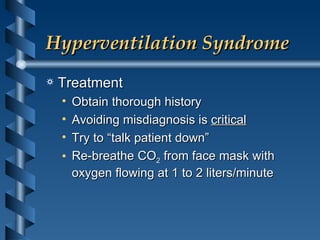
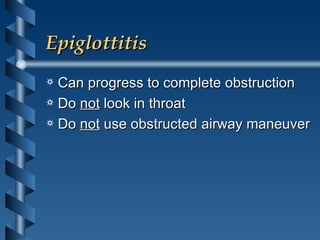
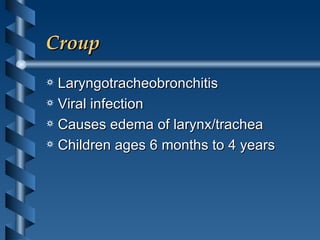
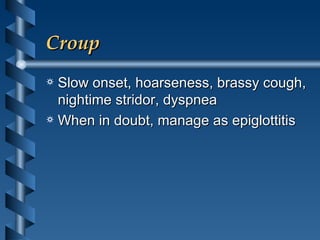
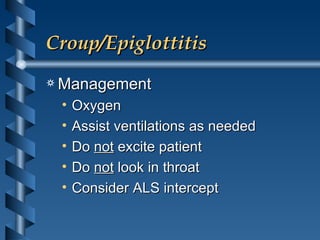
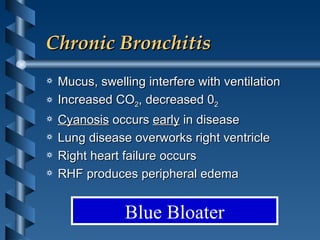
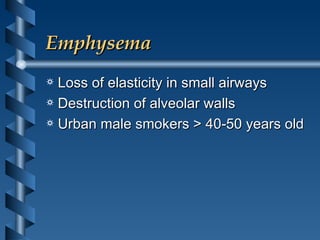
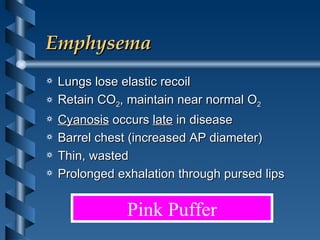
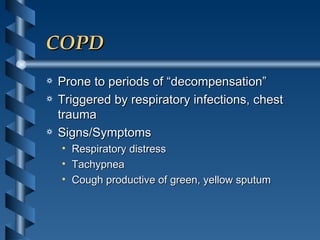
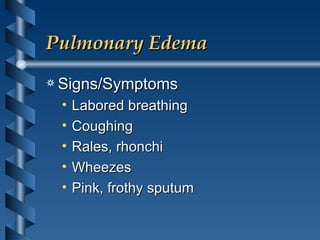
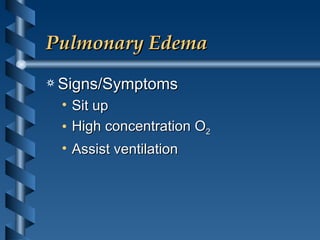
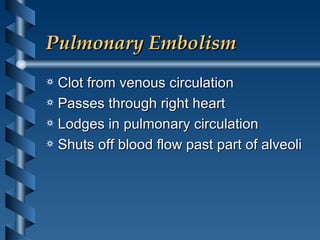
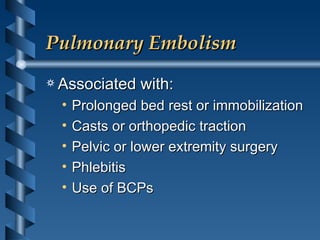
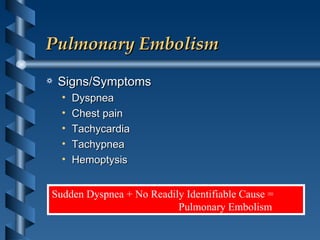
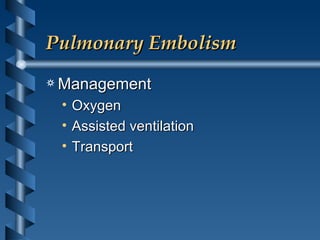
The document discusses various respiratory conditions that can cause dyspnea (difficult or labored breathing). It describes hyperventilation syndrome, which causes anxiety and dizziness due to overbreathing. Foreign body obstruction is a common cause of pediatric airway issues and can cause sudden dyspnea in adults. Pharyngeal edema, epiglottitis, and croup can cause upper airway swelling and obstruction. Asthma is a reversible obstructive lung disease often caused by allergens or irritants. Chronic obstructive pulmonary disease (COPD) includes chronic bronchitis and emphysema from long-term smoking. Pulmonary edema and pulmonary embolism can cause fluid or clots in the lungs resulting in