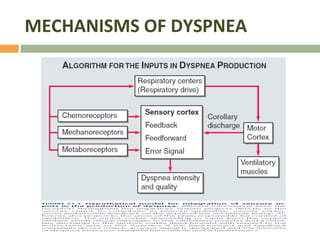
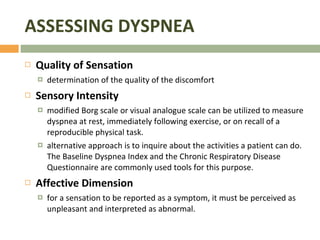
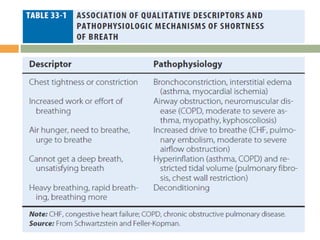
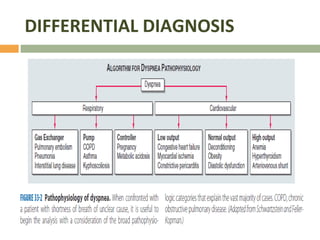
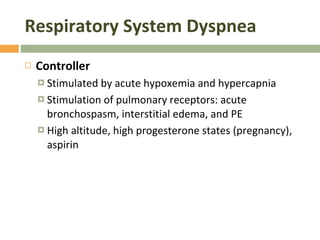
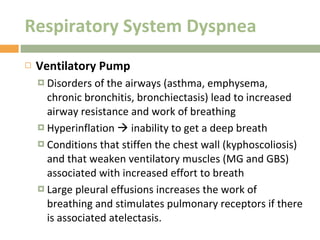
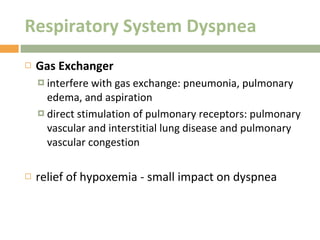
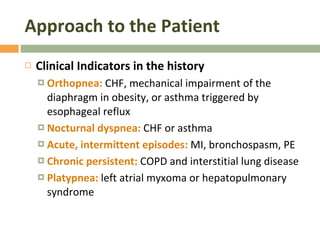
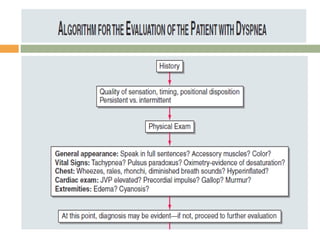
1) Dyspnea, or shortness of breath, is a subjective experience that results from interactions between physiological, psychological, and environmental factors. It can be caused by disorders of the ventilatory pump or sensory receptors in the lungs and muscles.
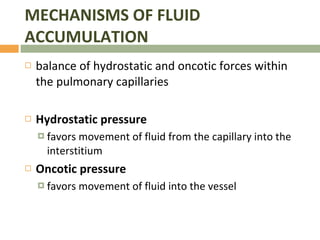
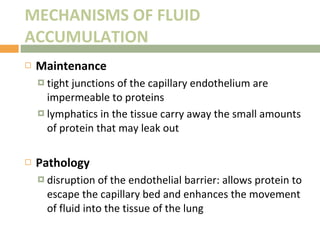
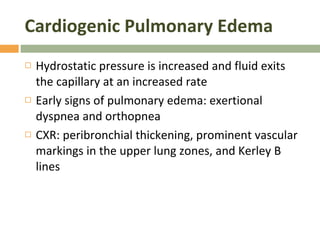
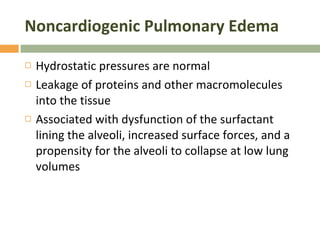
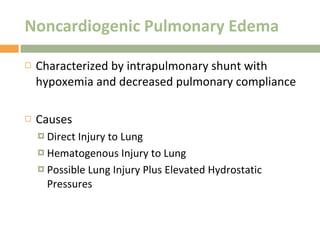
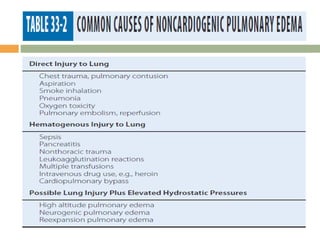
2) Pulmonary edema occurs when fluid accumulates in the lungs, which can be cardiogenic due to increased hydrostatic pressures from heart problems, or noncardiogenic from direct lung injury or diseases affecting the lung barrier.
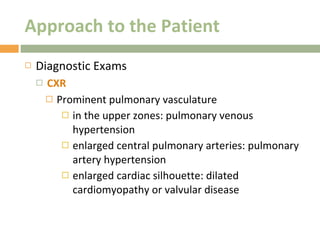
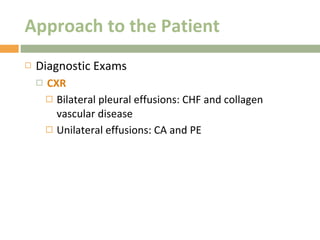
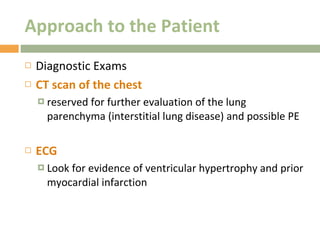
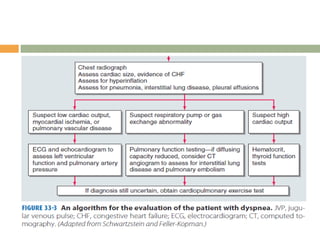
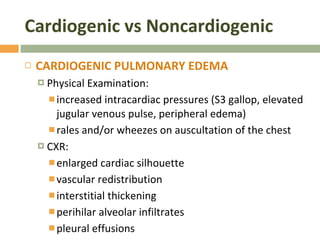
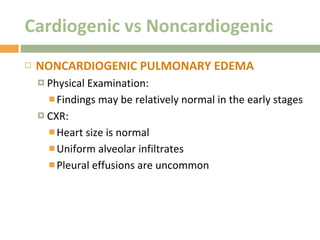
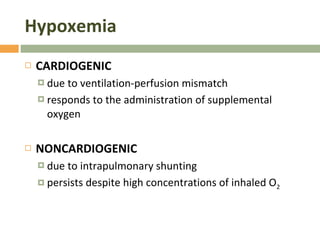
3) Differentiating cardiogenic and noncardiogenic pulmonary edema involves examining physical exam findings, chest x-rays, and response to supplemental oxygen, as they have distinct mechanisms and presentations.