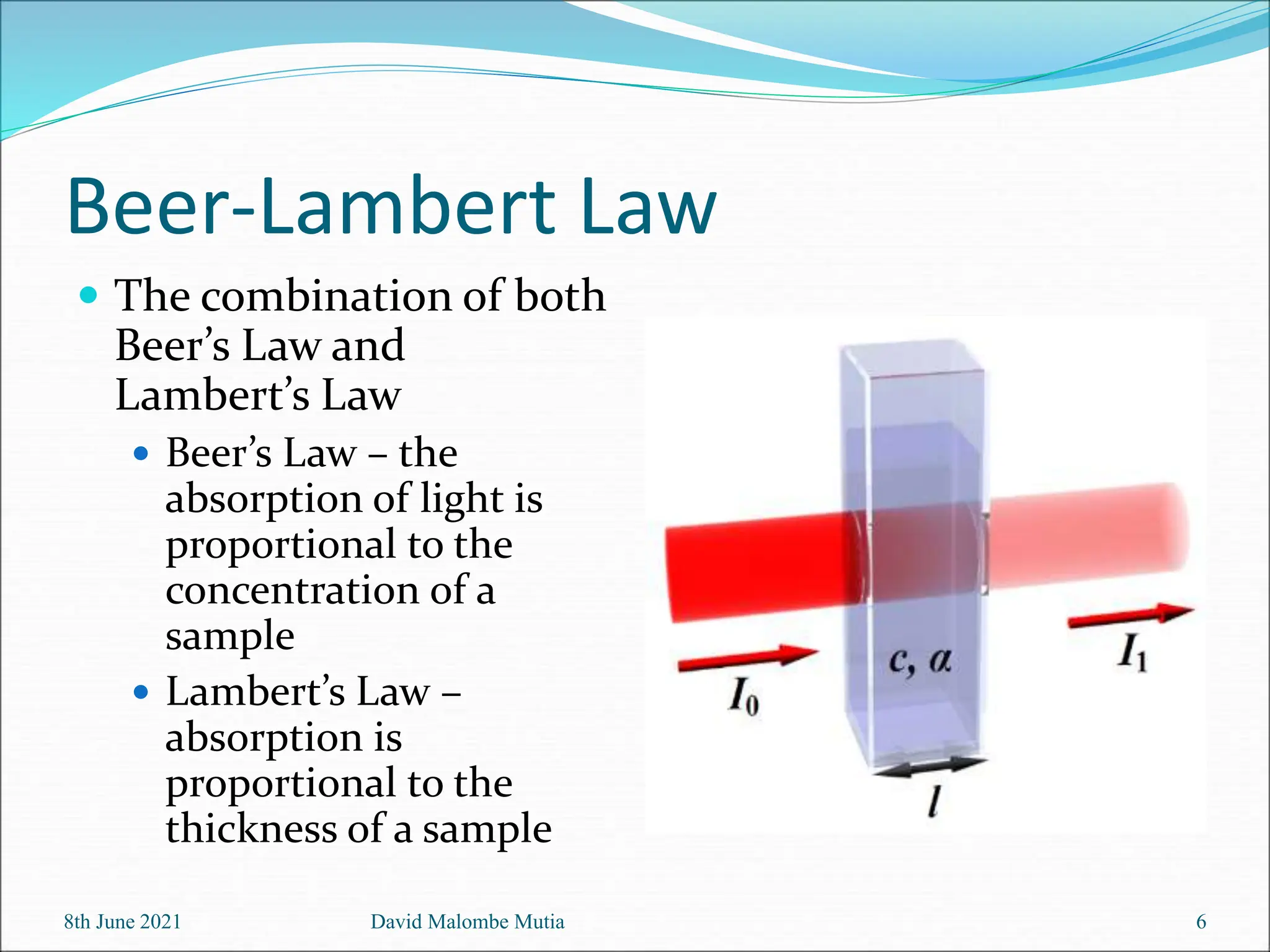
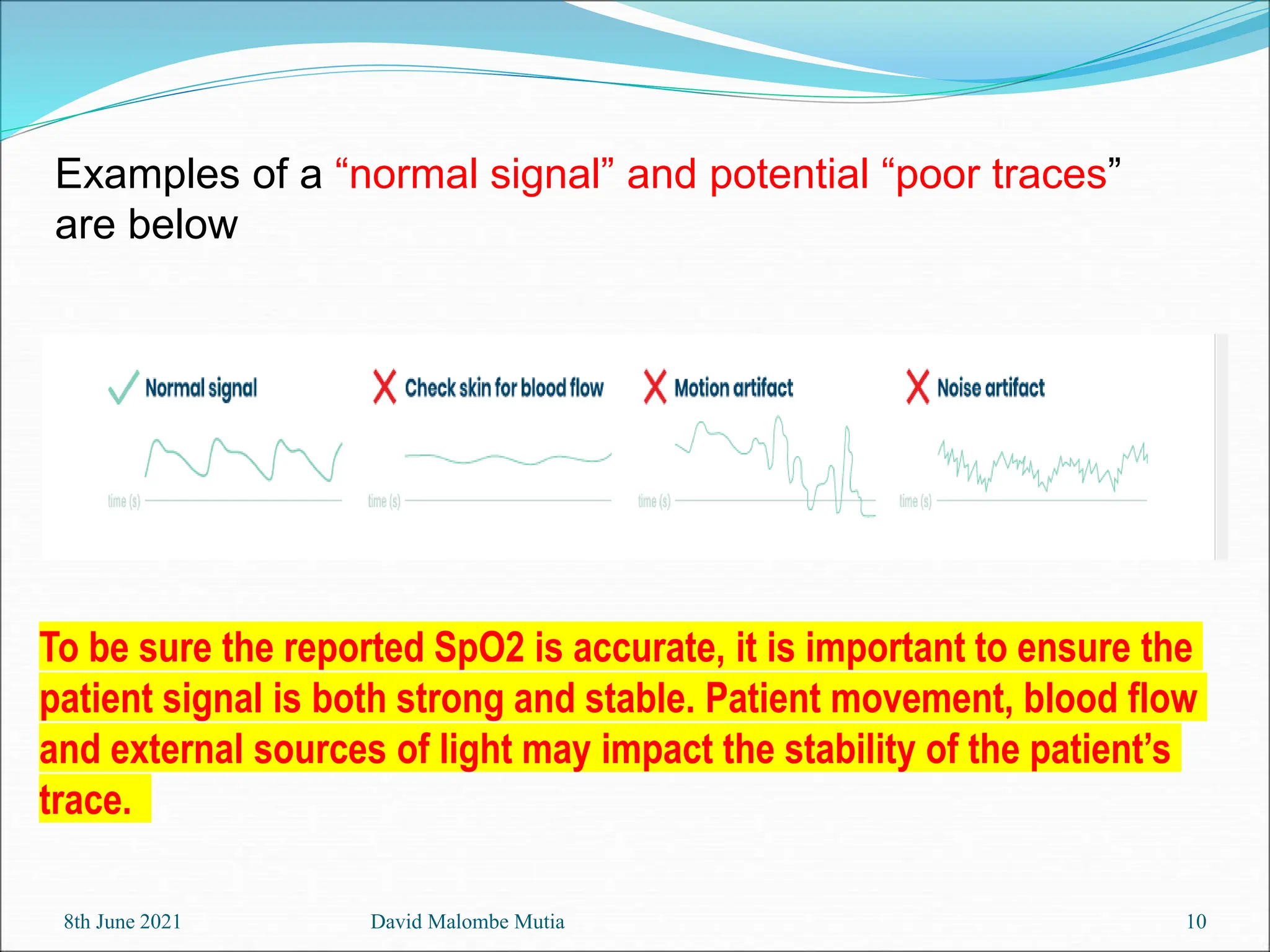
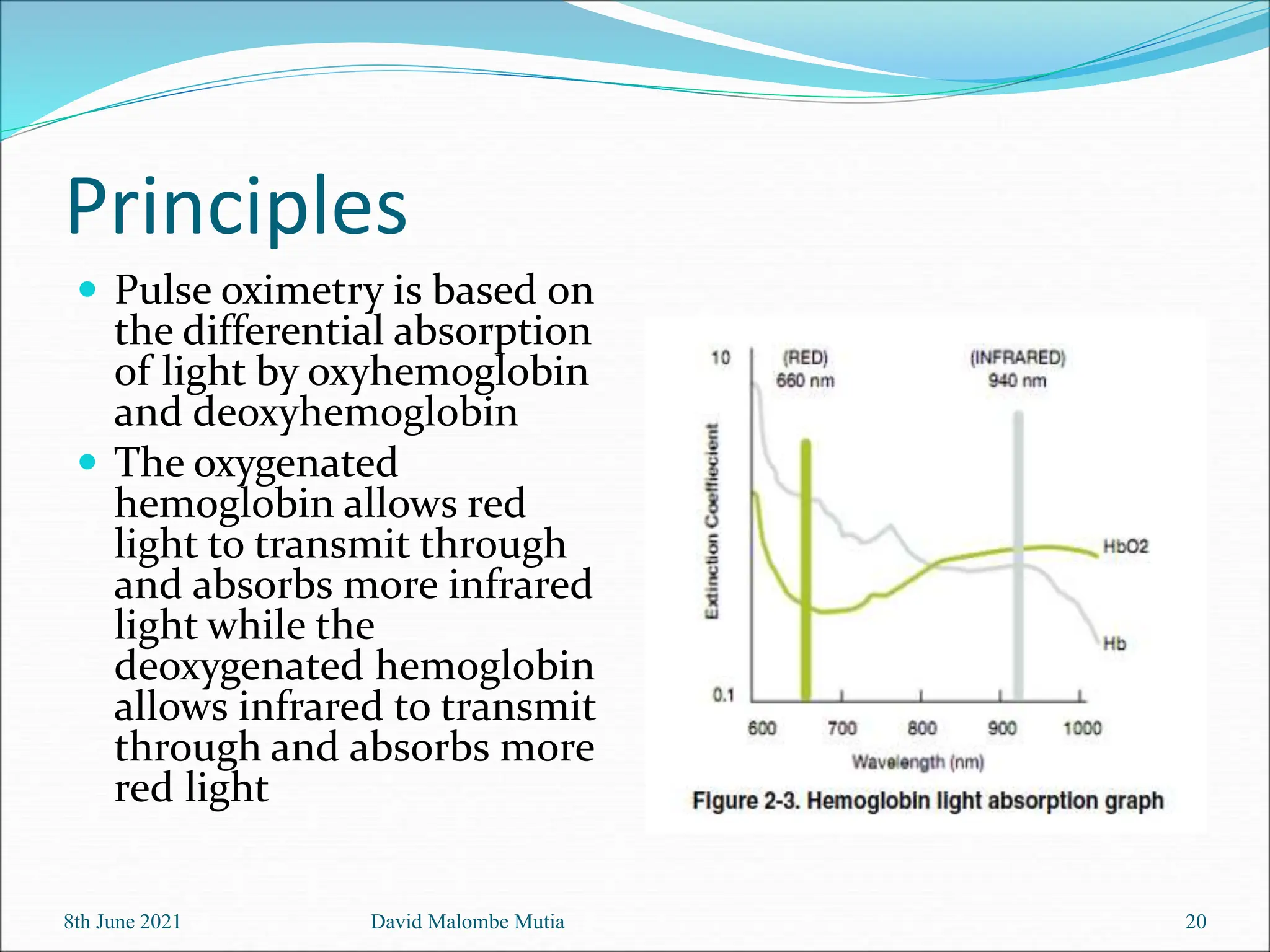
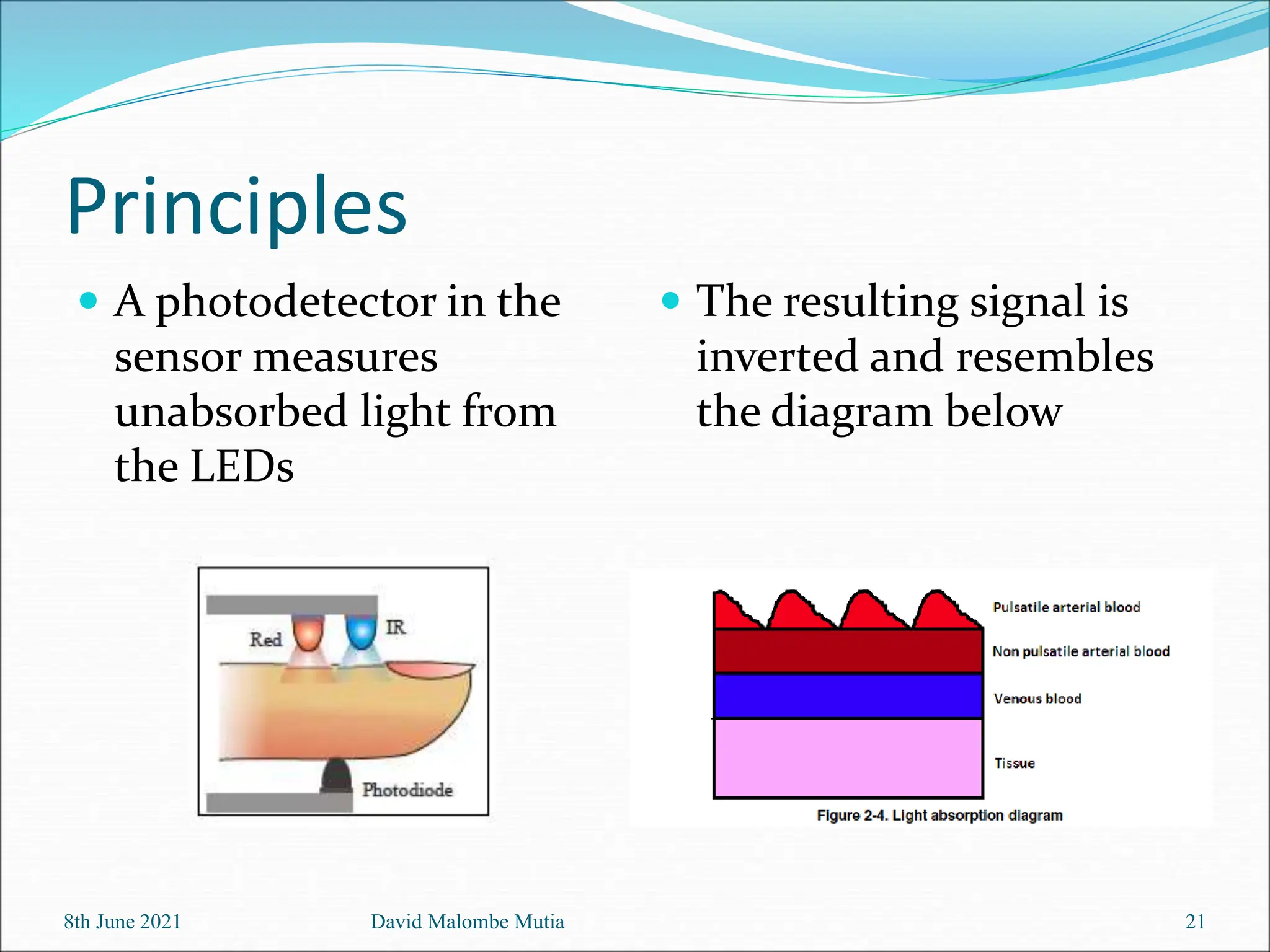
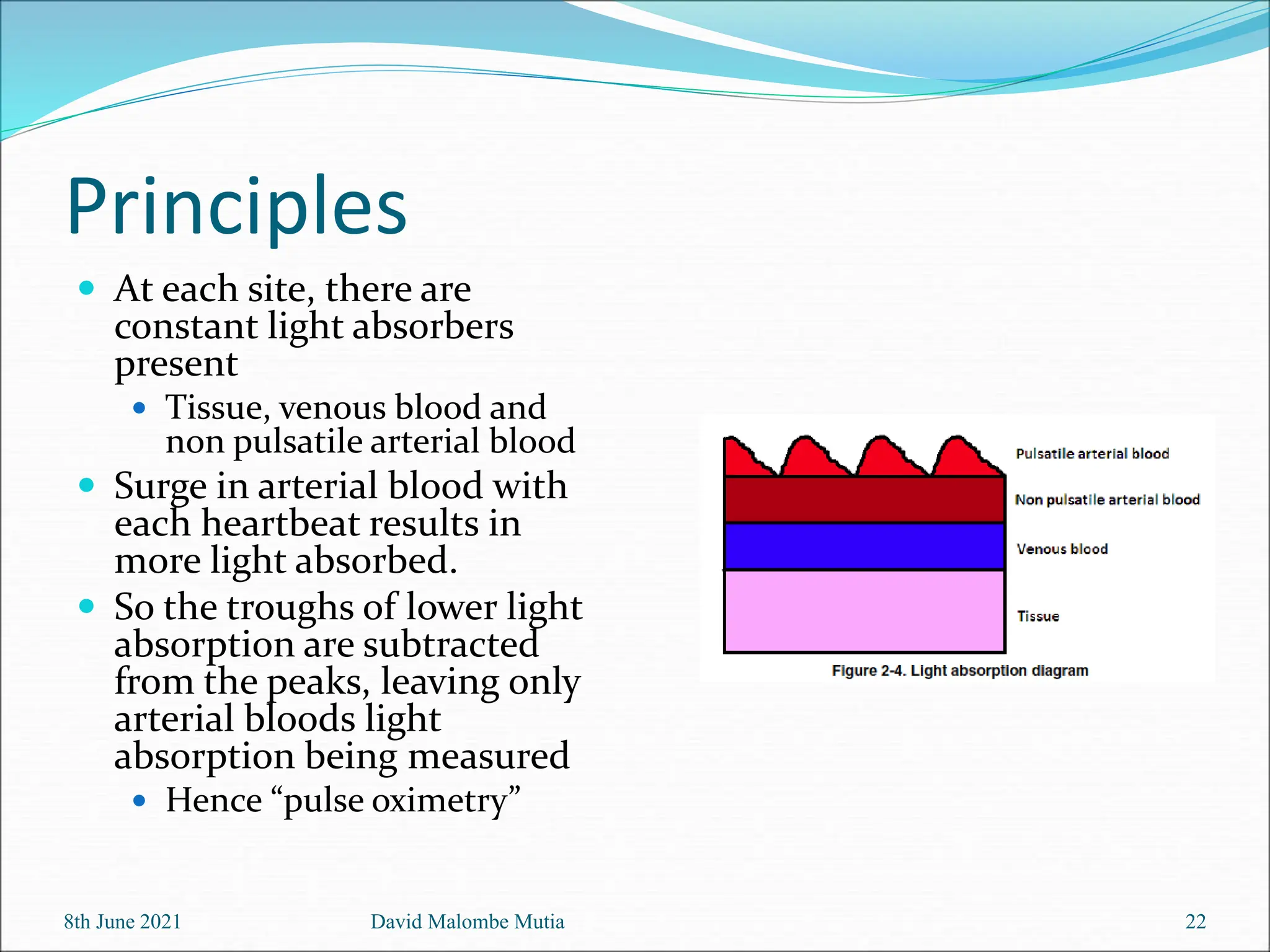
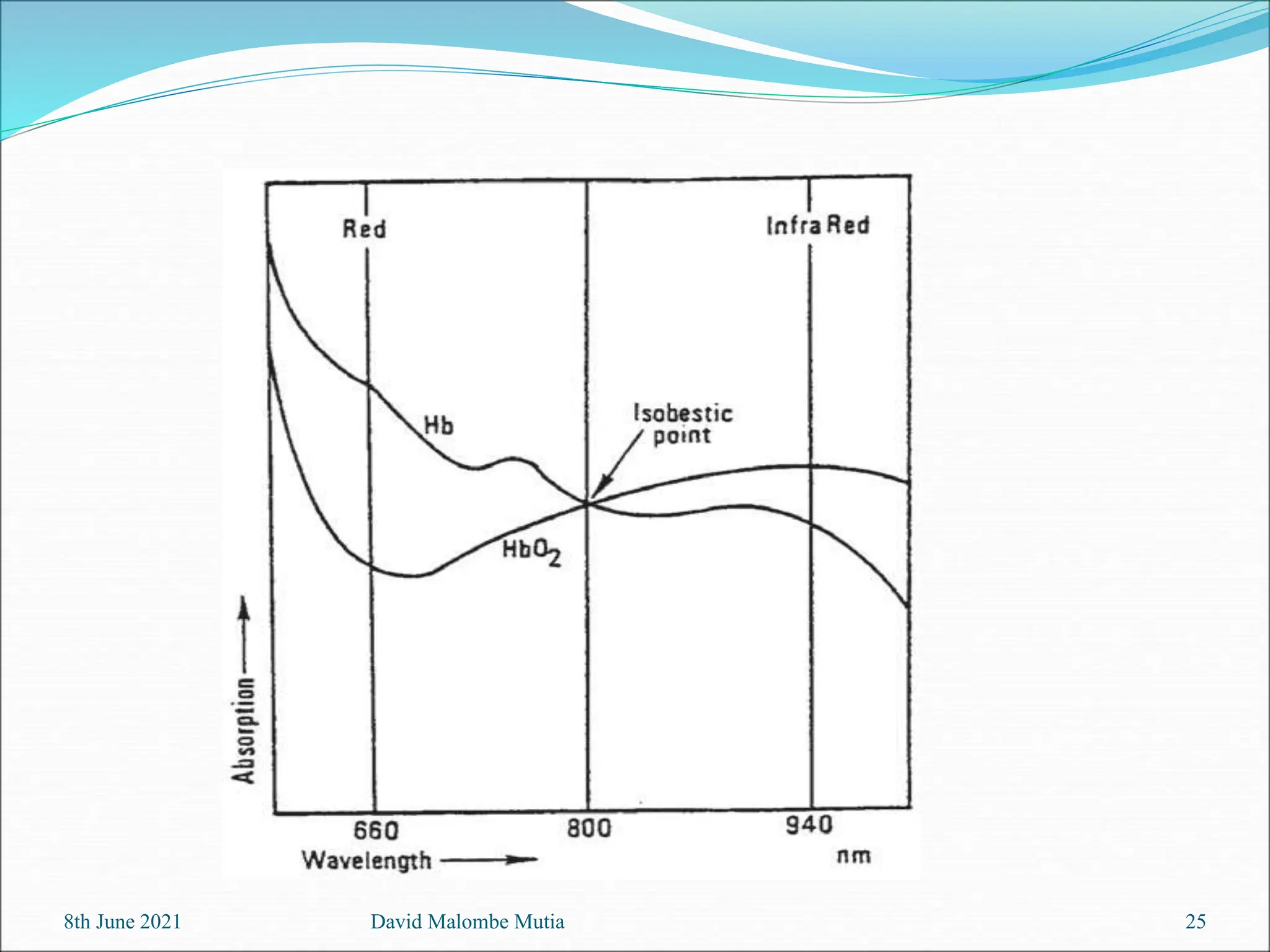
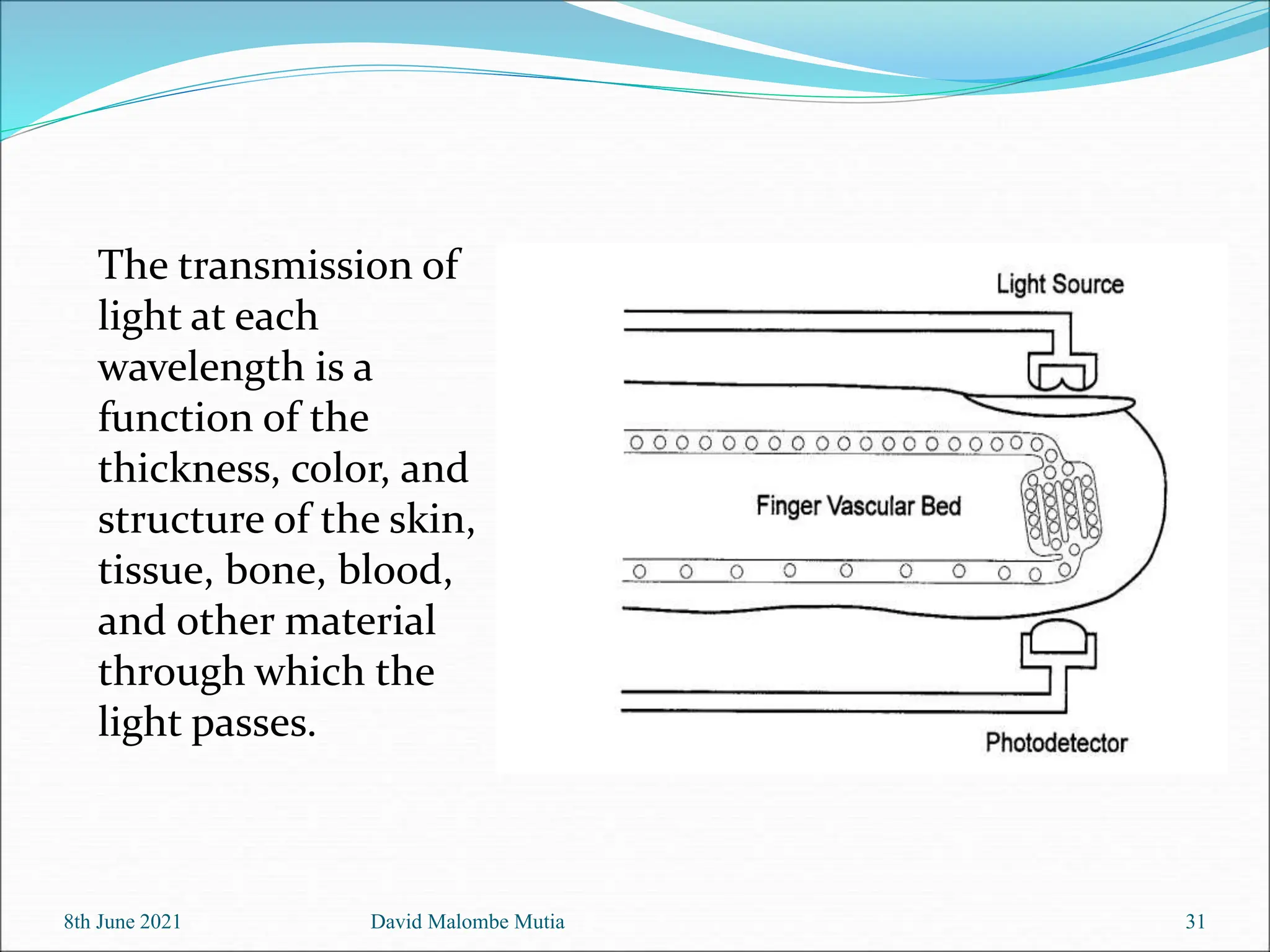
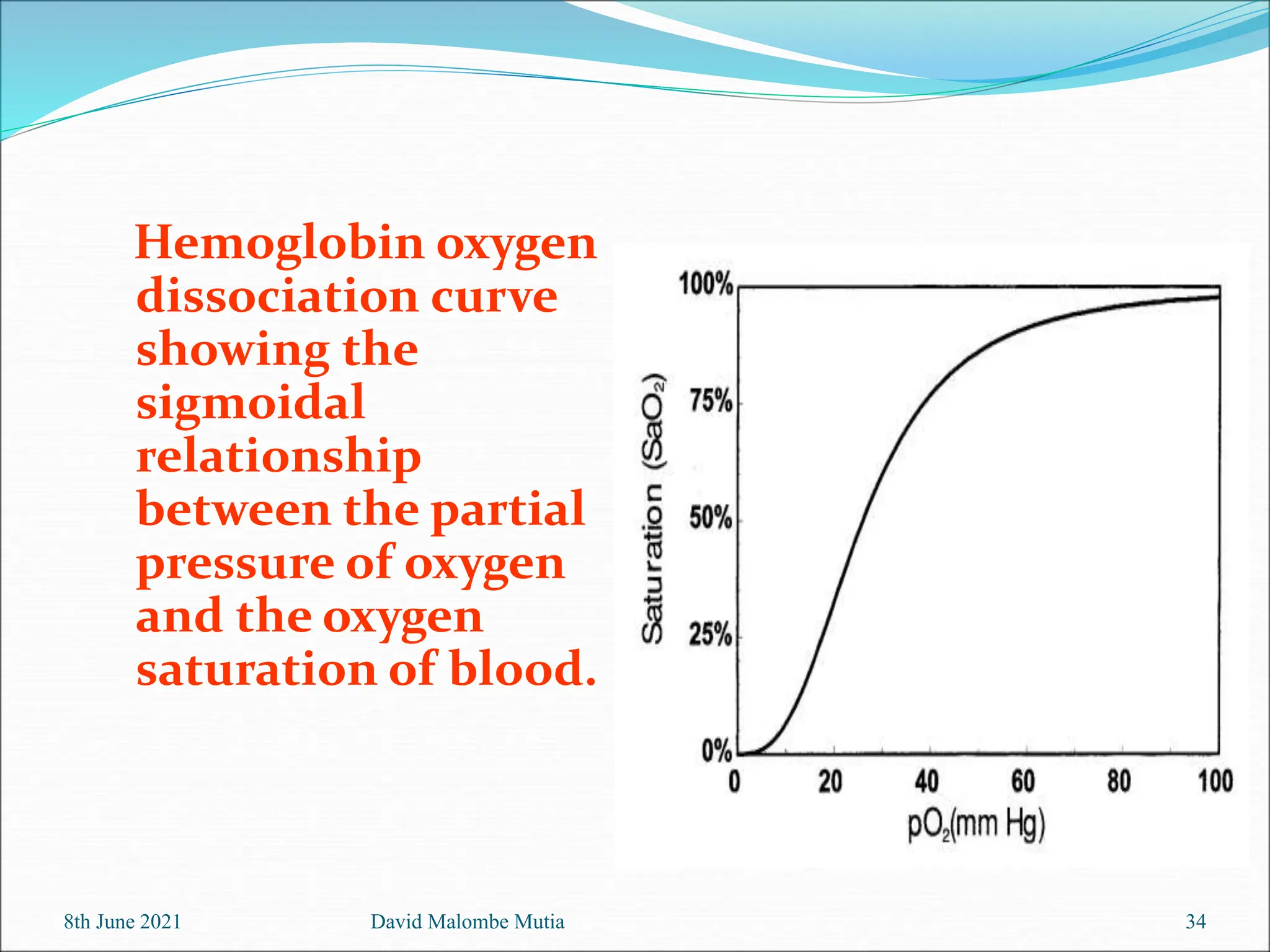
The document provides a comprehensive overview of pulse oximetry, detailing its aims, applications, principles, and historical development. It explains how pulse oximeters work, their construction, and the significance of blood oxygen saturation measures for patient health. It also discusses common sources of error when using pulse oximetry, emphasizing its advantages in noninvasive monitoring of oxygenation.