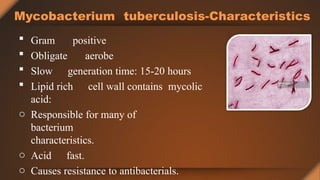
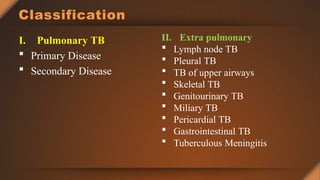
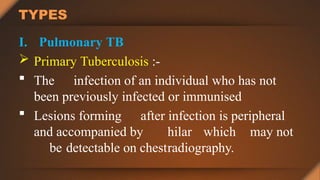
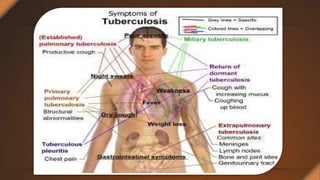
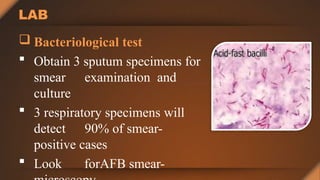
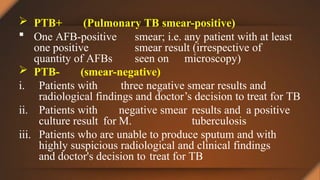
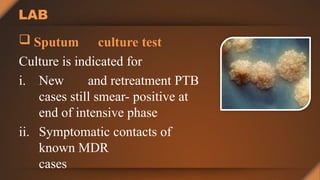
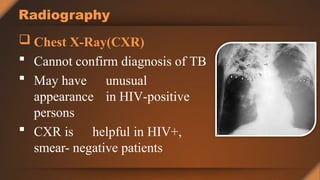
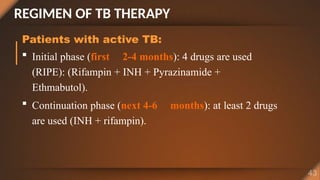
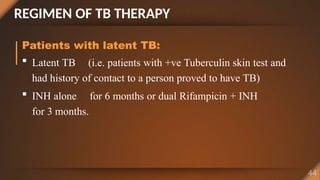
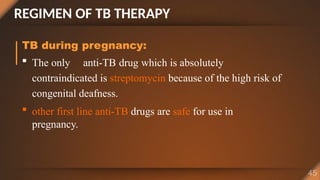
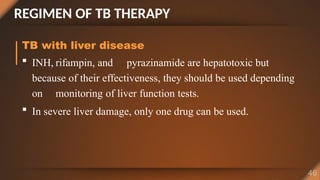
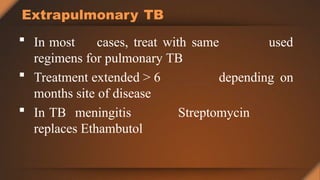
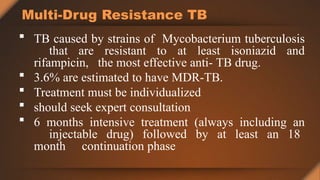
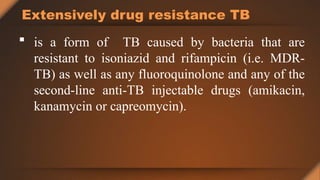
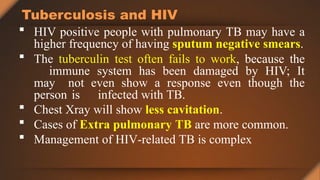
The document is a comprehensive overview of tuberculosis (TB), a contagious disease primarily affecting the lungs, with significant global health implications, such as causing 1.6 million deaths annually. It outlines the causes, types, risk factors, diagnosis, and treatment options for TB, highlighting the challenges posed by multidrug-resistant strains. It also emphasizes the importance of careful management, especially for patients with coexisting HIV infections.