This document summarizes key aspects of pulmonary tuberculosis, including:
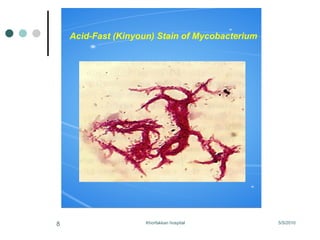
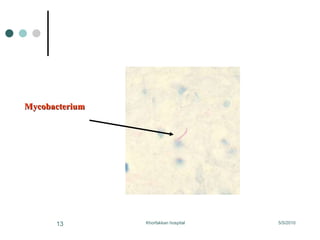
1. Pulmonary tuberculosis is diagnosed by considering TB in the differential diagnosis when symptoms are present and ordering appropriate diagnostic tests.
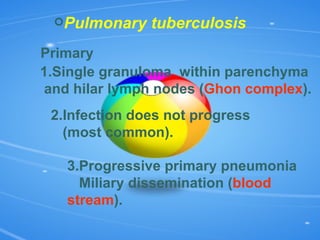
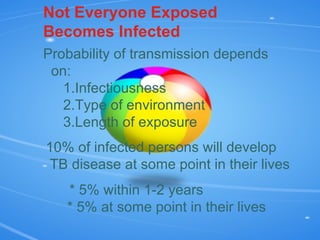
2. Factors like decreased cough reflex and impaired immune function can allow tuberculosis bacteria to infect the lungs and spread.
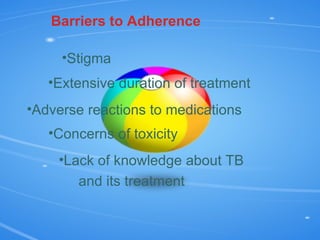
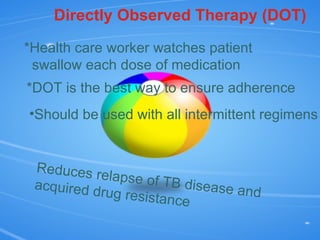
3. Treatment requires a multi-drug regimen administered under direct observation to ensure adherence and prevent drug resistance, as non-adherence can allow the disease to relapse or spread.