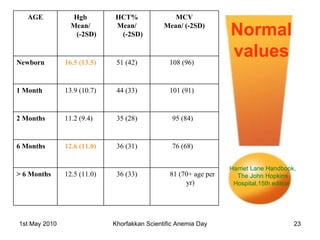
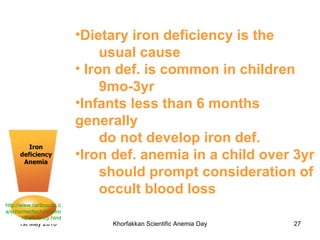
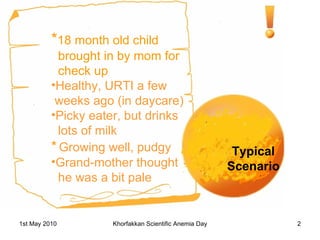
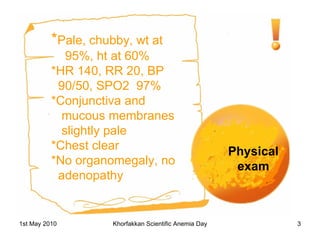
1. The document discusses a case of childhood iron deficiency anemia in an 18-month old child who presents with pale skin and fatigue.
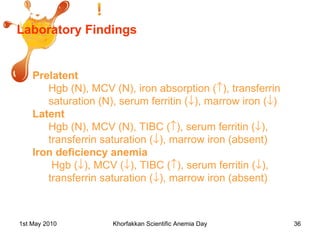
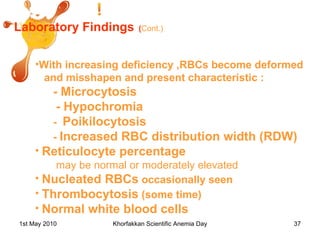
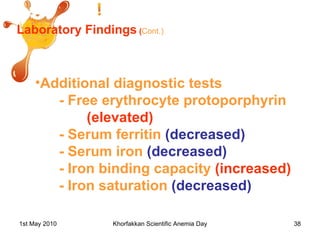
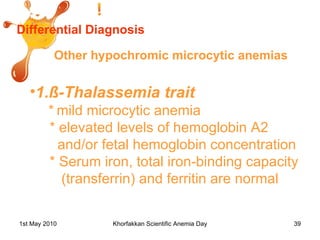
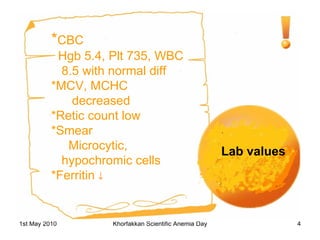
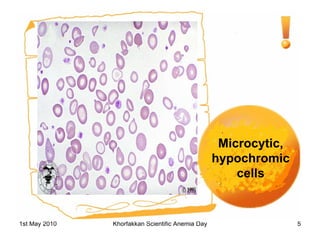
2. Laboratory tests confirm the diagnosis of iron deficiency anemia through low hemoglobin and iron levels.
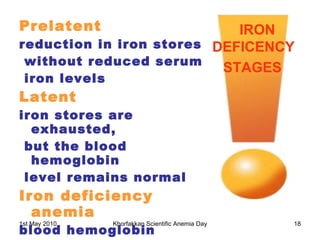
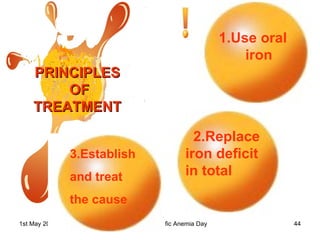
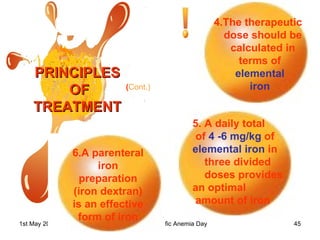
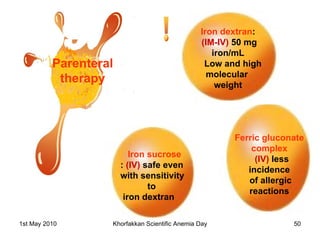
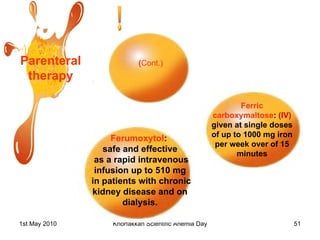
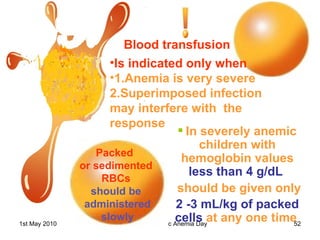
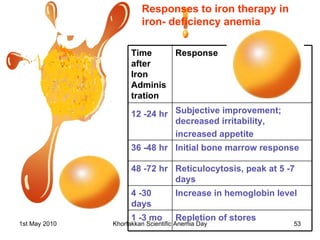
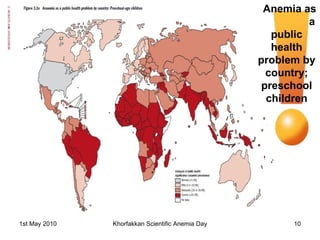
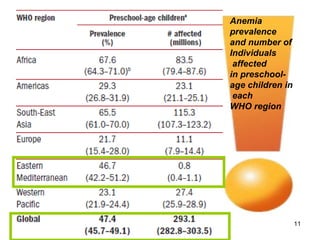
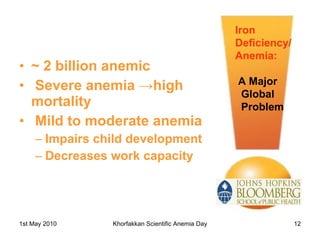
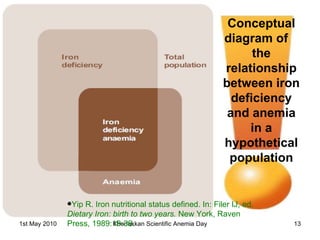
3. Iron deficiency anemia is a major global health problem, affecting over 2 billion people worldwide, especially preschool children in developing countries. Treating the underlying cause and replacing iron stores orally or parenterally is important for management.
![WHO Diagnosis Hemoglobin below 11gm/dl in pre school children. ANEMIA UNICEF/UNU/WHO. Iron deficiency anemia: assessment, prevention and control. A guide for programme managers.WHO/NHD,2001 [report no.01.3]](https://image.slidesharecdn.com/childhoodida2010-100518131836-phpapp02/85/Childhood-ida2010-15-320.jpg)