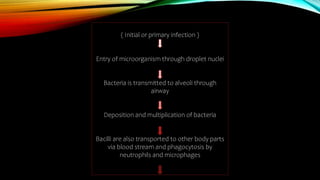
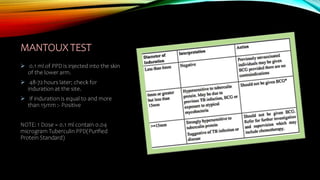
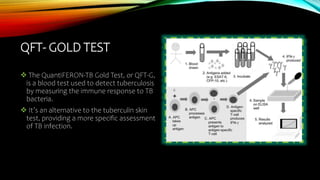
The document is a comprehensive slide deck on tuberculosis (TB), covering its history, incidence, types, risk factors, clinical manifestations, and management strategies. It outlines the importance of early diagnosis and treatment, including Directly Observed Treatment Short Course (DOTS) and various anti-tubercular drugs. The document emphasizes the ongoing global health challenge of TB and the need for improved healthcare initiatives to combat it.