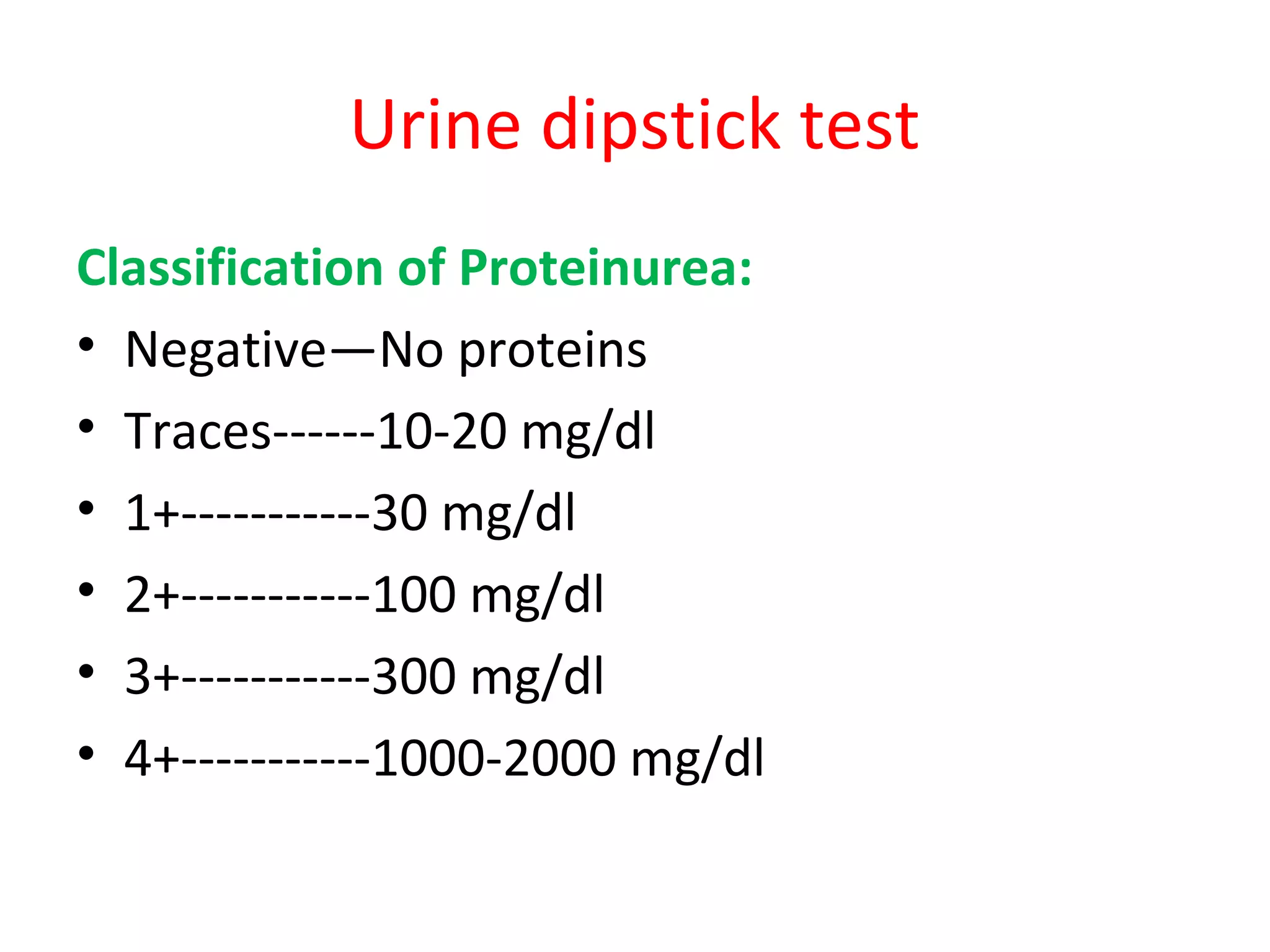
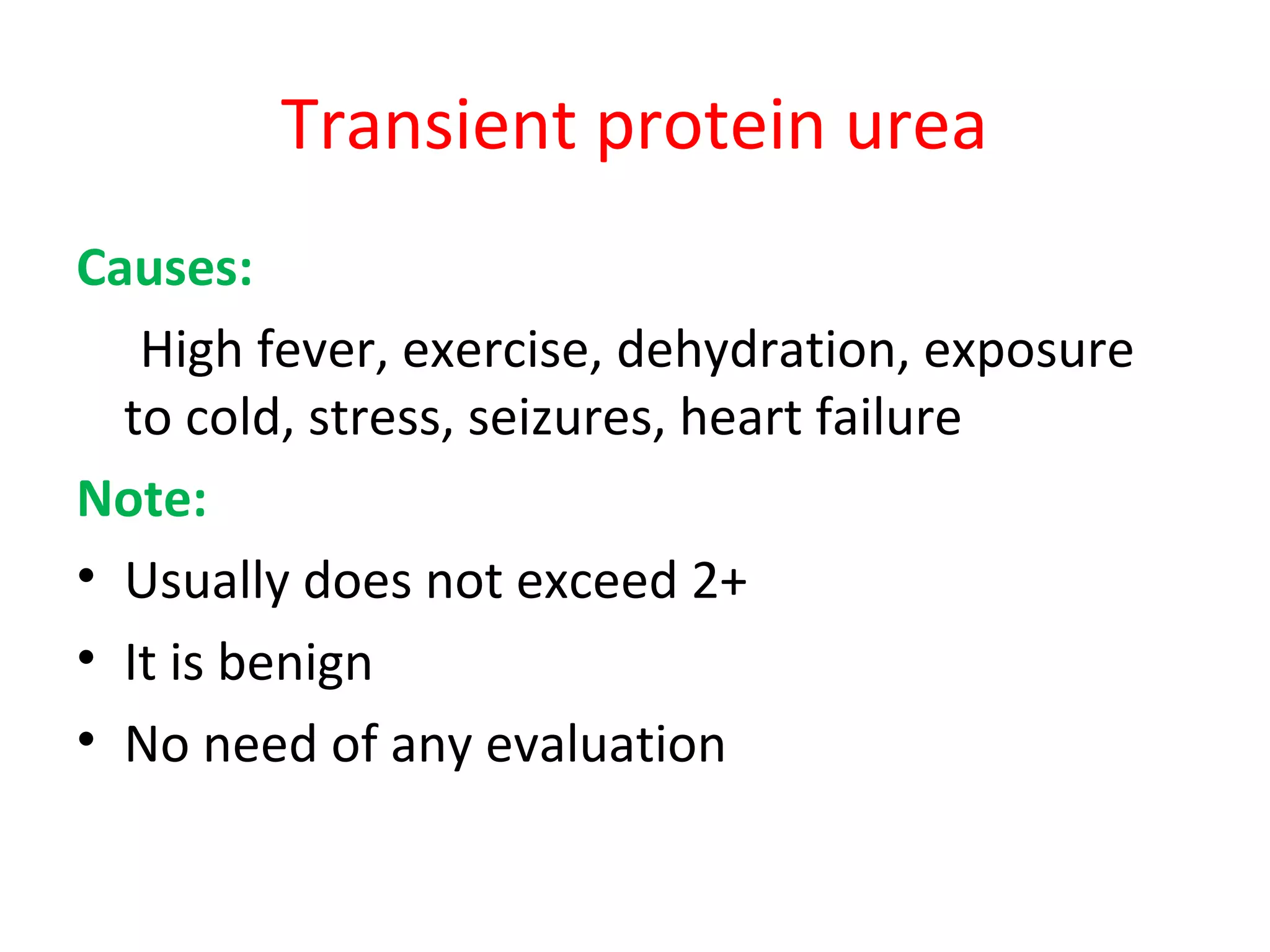
Proteinuria and nephrotic syndrome can be diagnosed through urine dipstick testing, urinary protein to creatinine ratio, and 24-hour urine collection. Minimal change nephrotic syndrome is the most common cause of nephrotic syndrome in children and is characterized by heavy proteinuria, hypoalbuminemia, edema, and hyperlipidemia. It is typically treated with steroid therapy, though some children are steroid resistant or dependent. Complications of nephrotic syndrome include increased risk of infection and thromboembolic events.