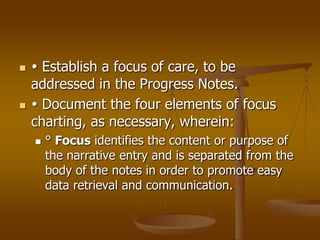
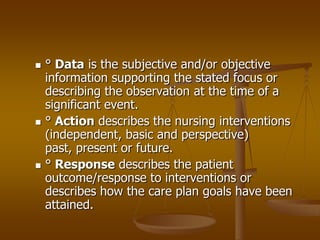
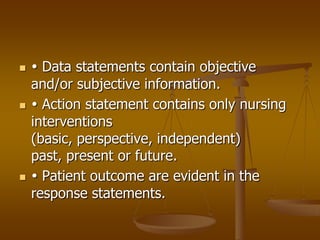
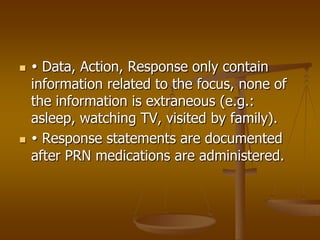
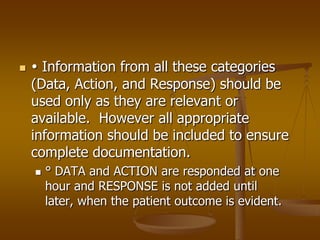
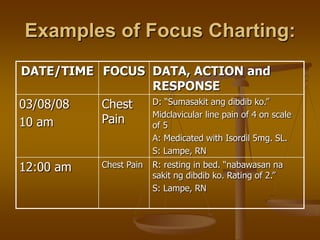
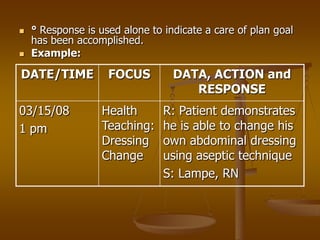
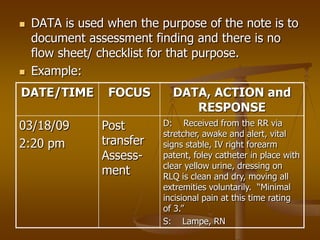
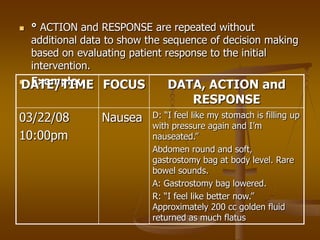
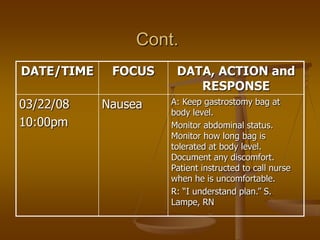
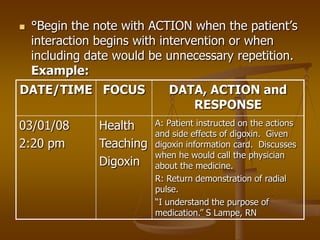
Focus charting describes documenting from the patient's perspective by focusing on their current status, progress towards goals, and response to interventions. It brings the focus back to the patient's concerns using a focus column that incorporates aspects of patient care instead of a problem list. The narrative portion of focus charting includes documenting Data, Action, and Response (DAR) to provide a holistic emphasis on the patient and their priorities.