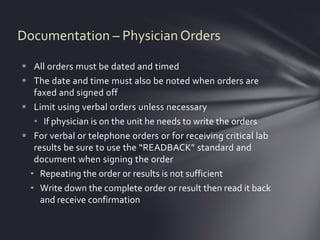
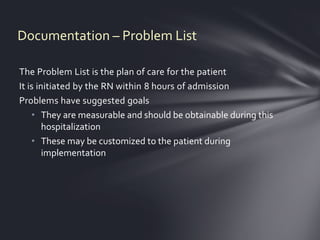
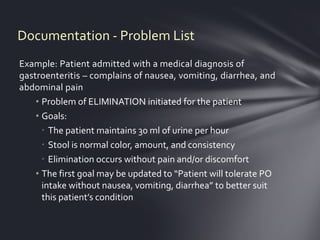
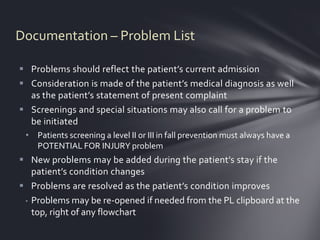
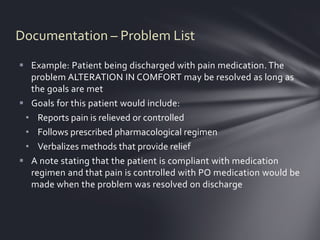
Nurses document patient care in the electronic medical record system. Documentation includes assessments, interventions, patient responses, medication administration, education provided, and routine checks. Physical assessments are done within 8 hours of admission and every shift, with problems addressed in the problem list. Orders are dated, timed, and read back to ensure accuracy. The problem list guides care and is updated as goals are met or conditions change.