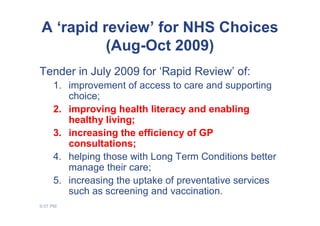
This document summarizes a rapid review conducted by Ray Jones on the impact of computer use by patients. The review was commissioned by NHS Choices to examine how digital health services can: 1) improve access to care and support choice; 2) improve health literacy and enable healthy living; 3) increase GP consultation efficiency; 4) help those with long-term conditions manage care; and 5) increase preventive service uptake like screening and vaccination. The review found evidence that e-health interventions can improve patients' health knowledge and attitudes in the short-term and potentially change health behaviors. However, most studies only show short-term behavior changes and there is limited evidence on sustained lifestyle improvements or health outcomes. Methodological challenges in evaluating e-