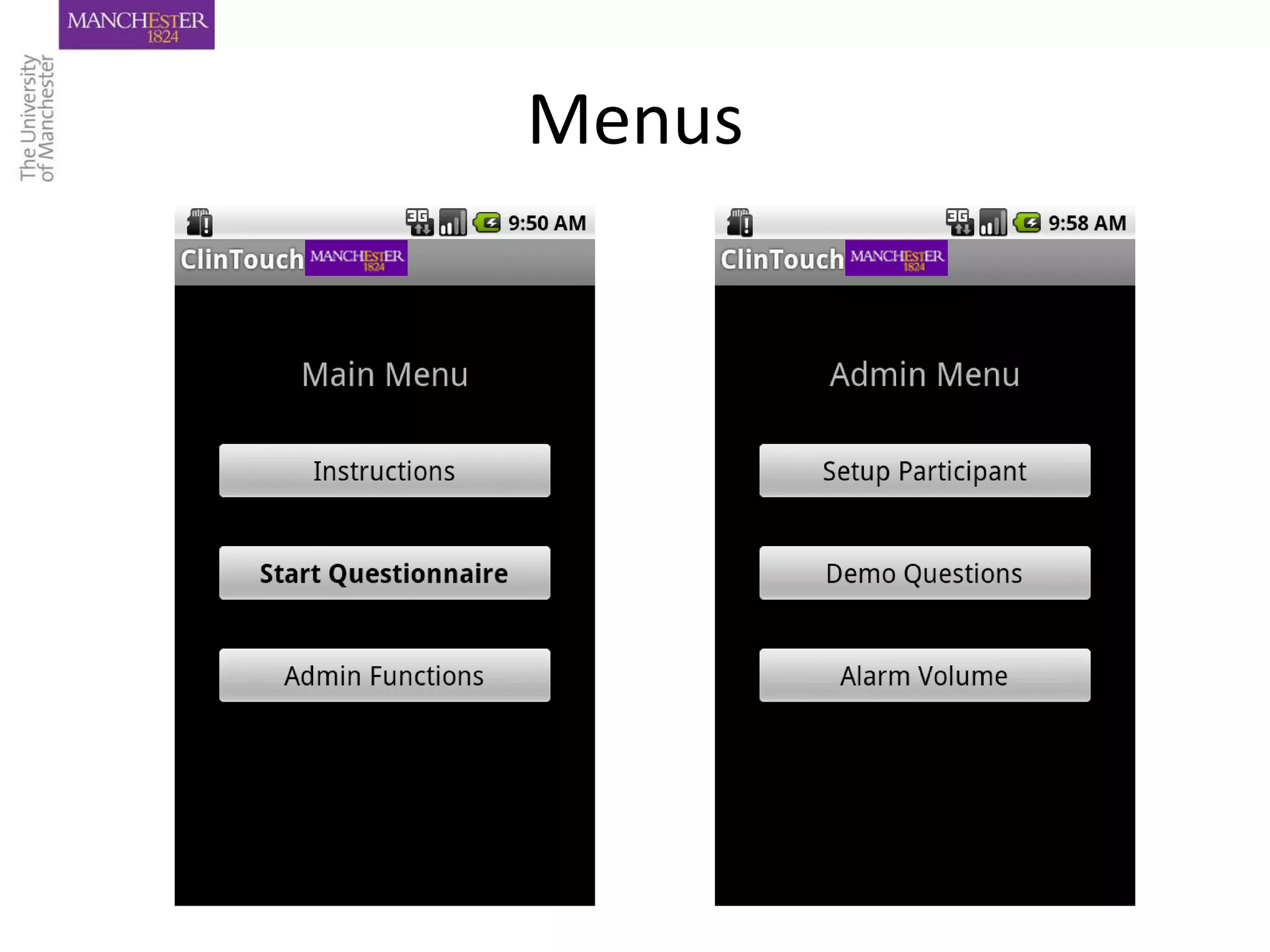
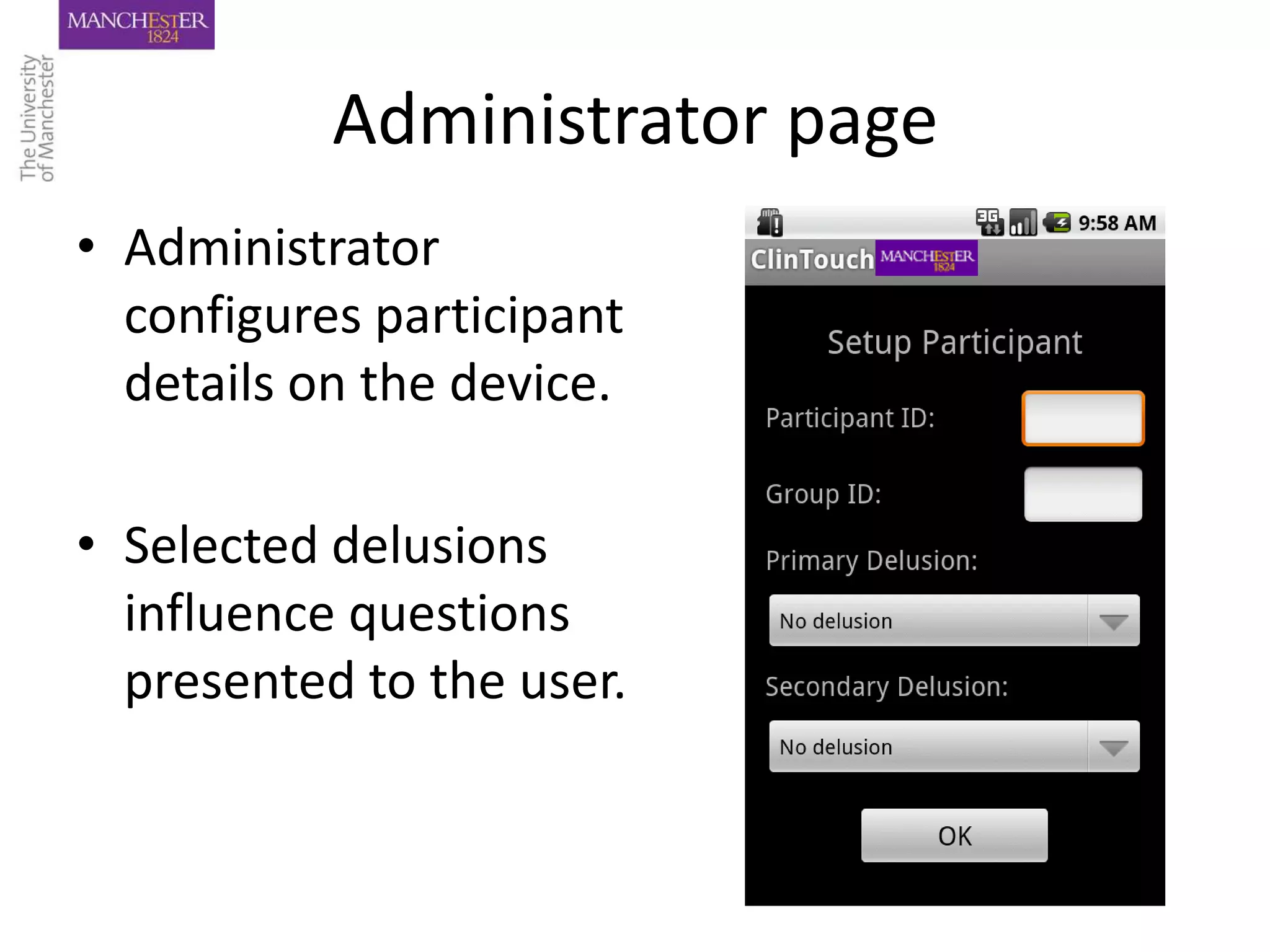
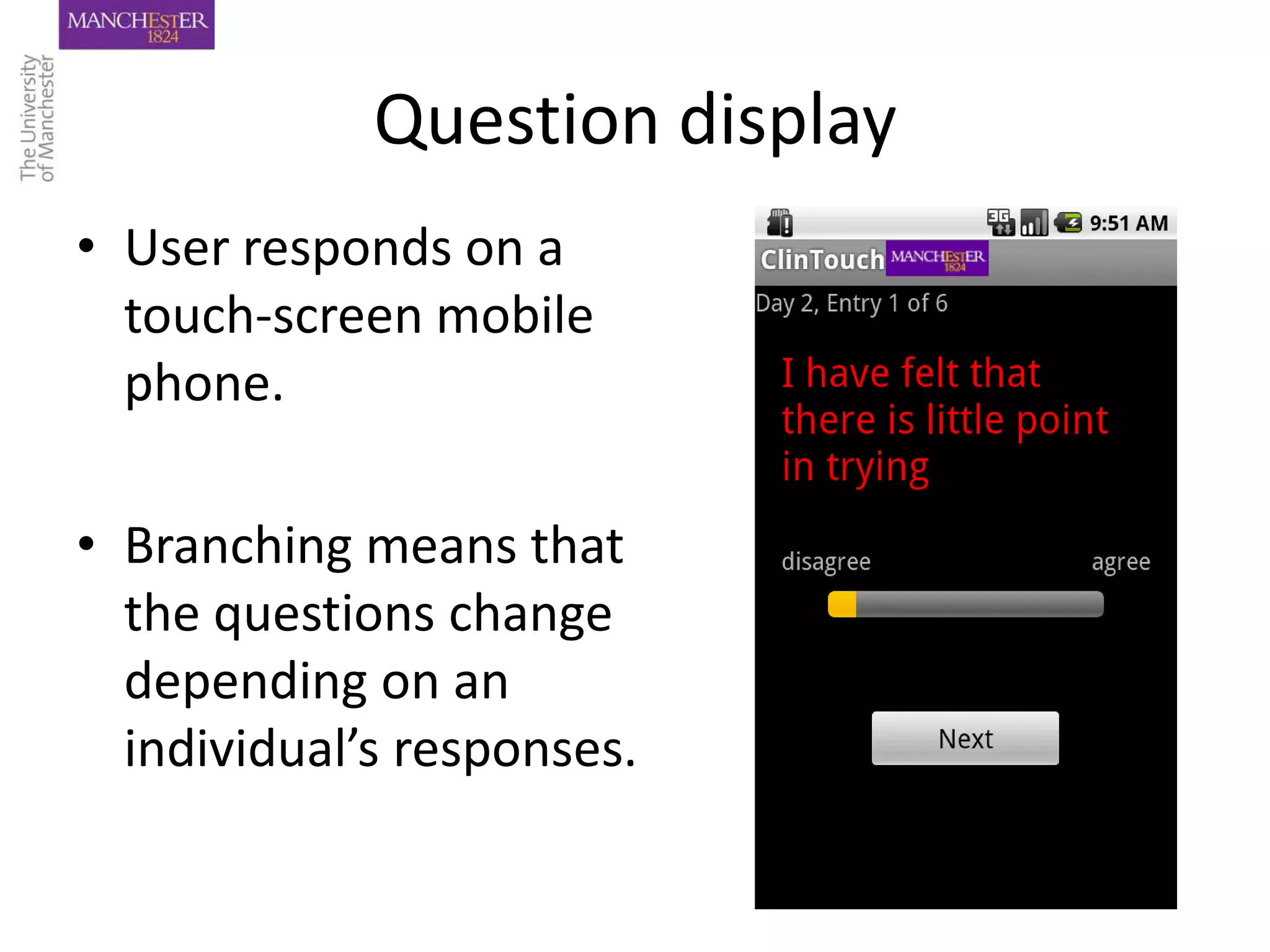
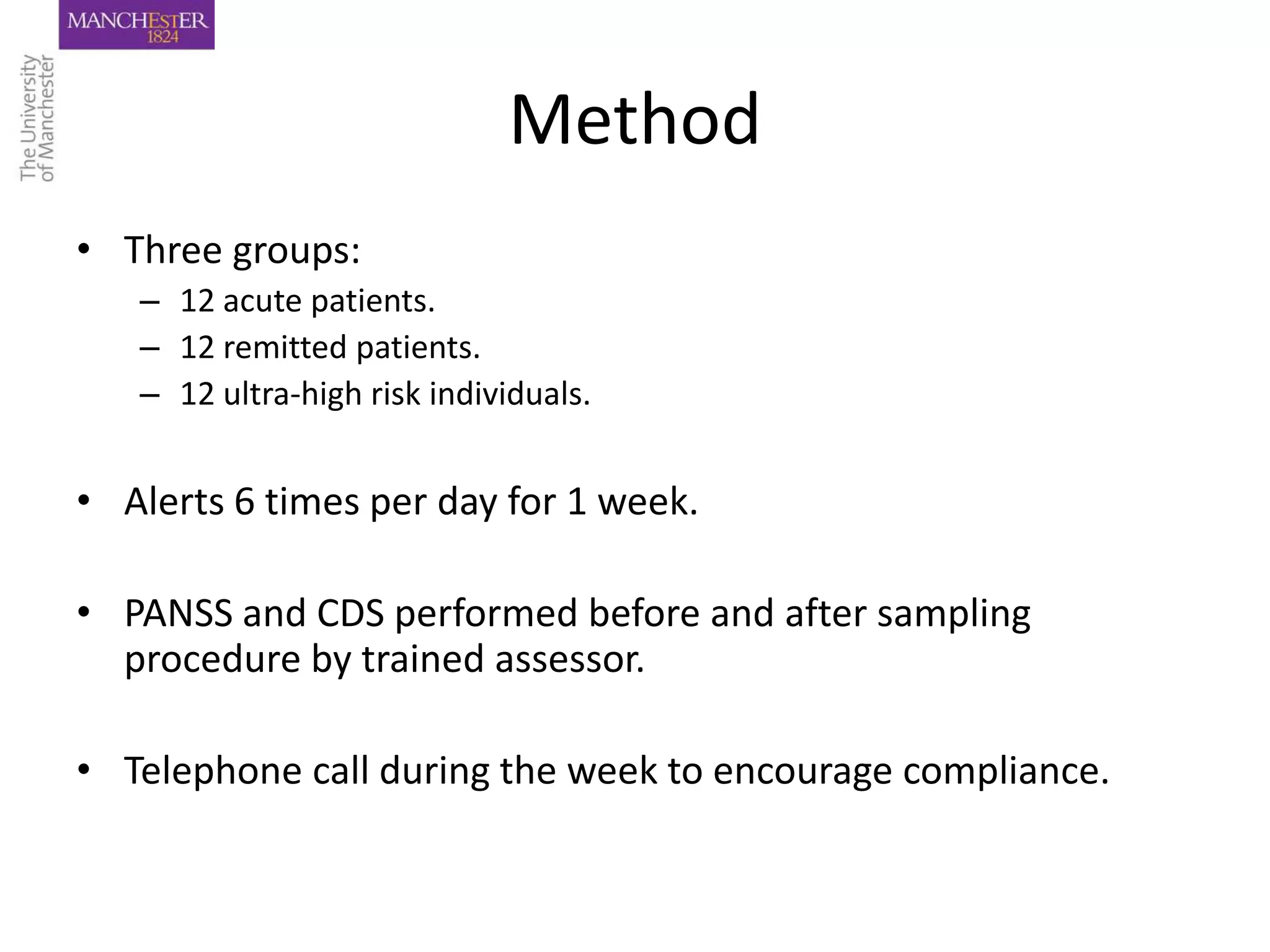
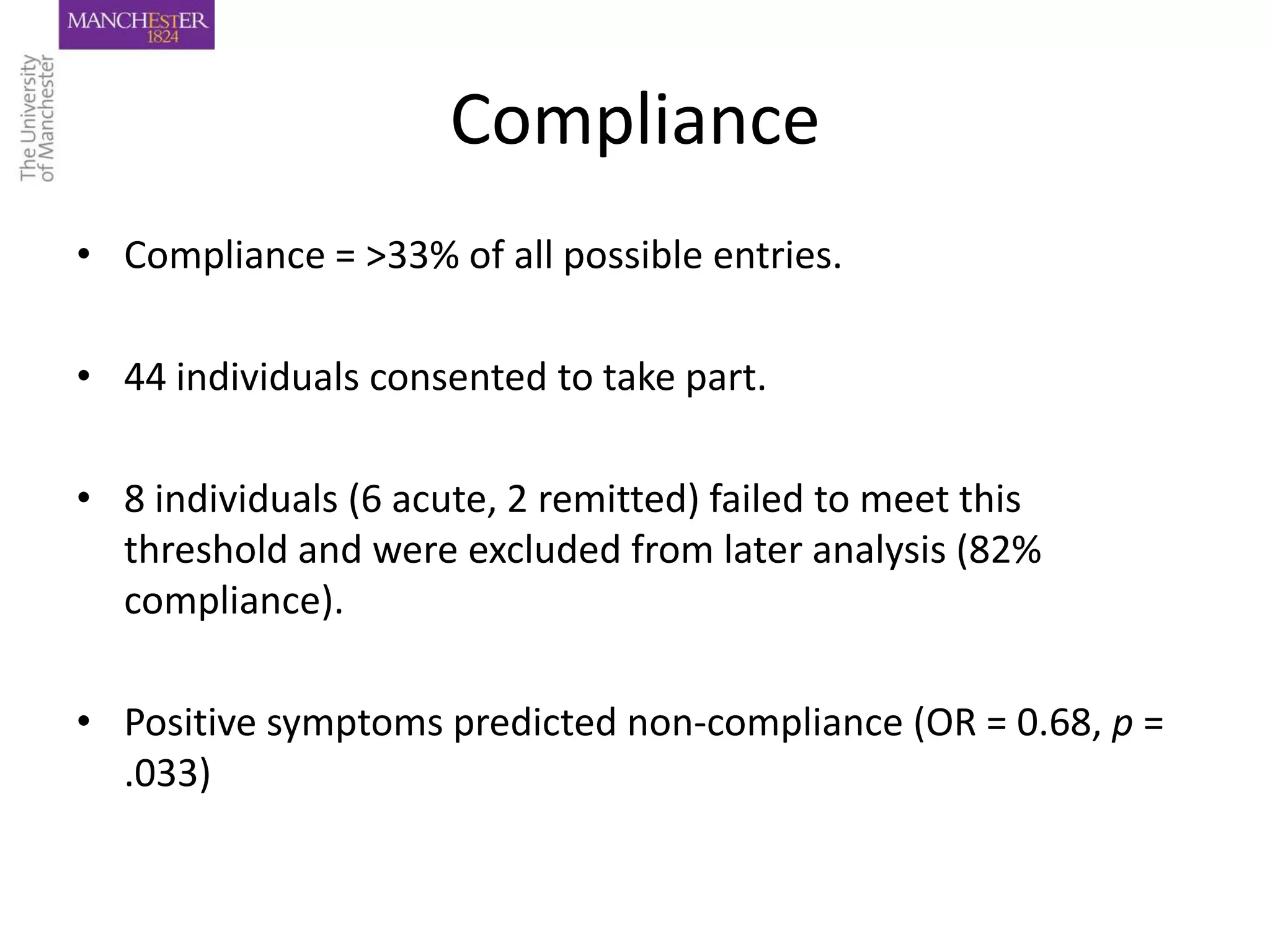
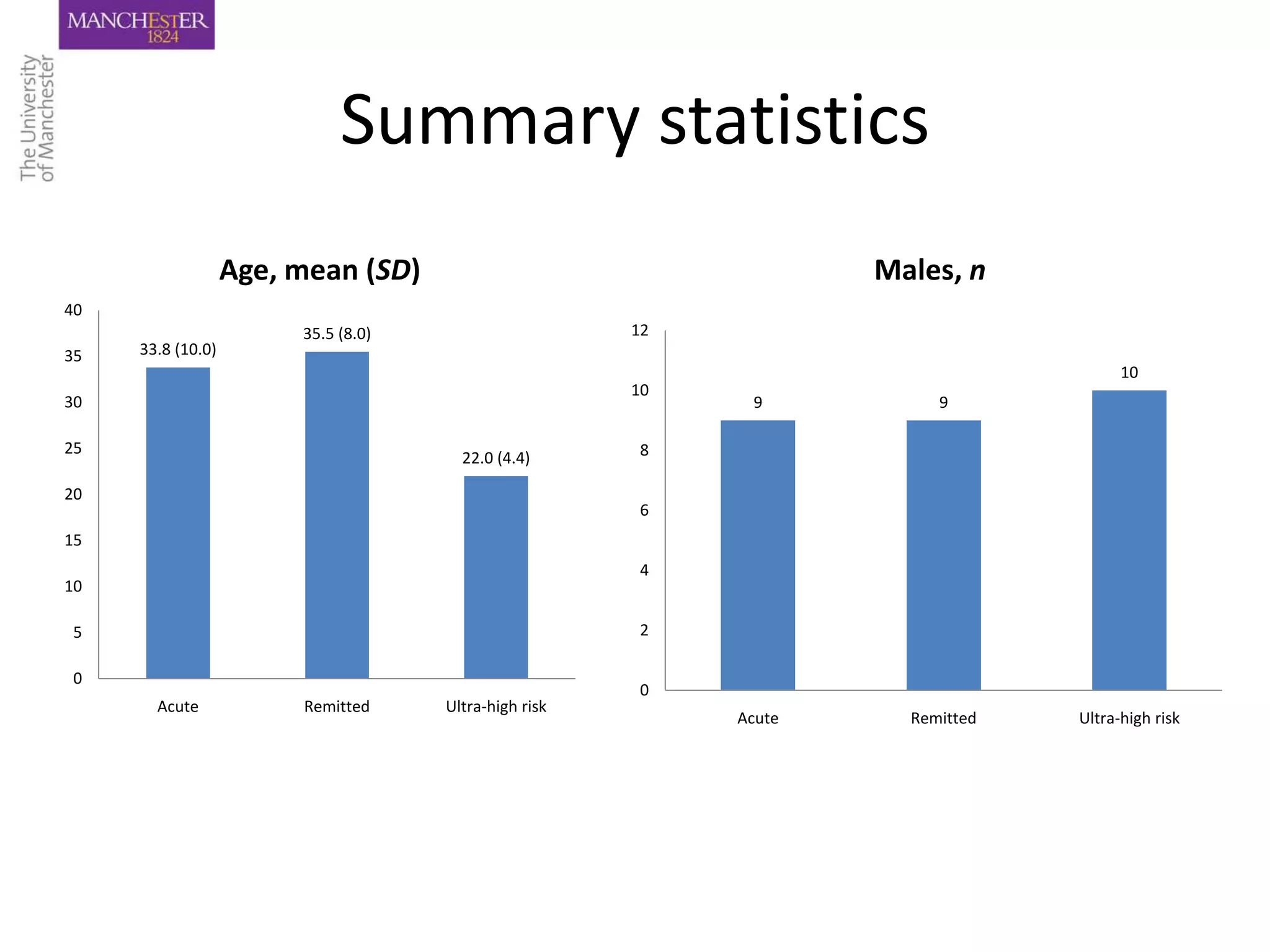
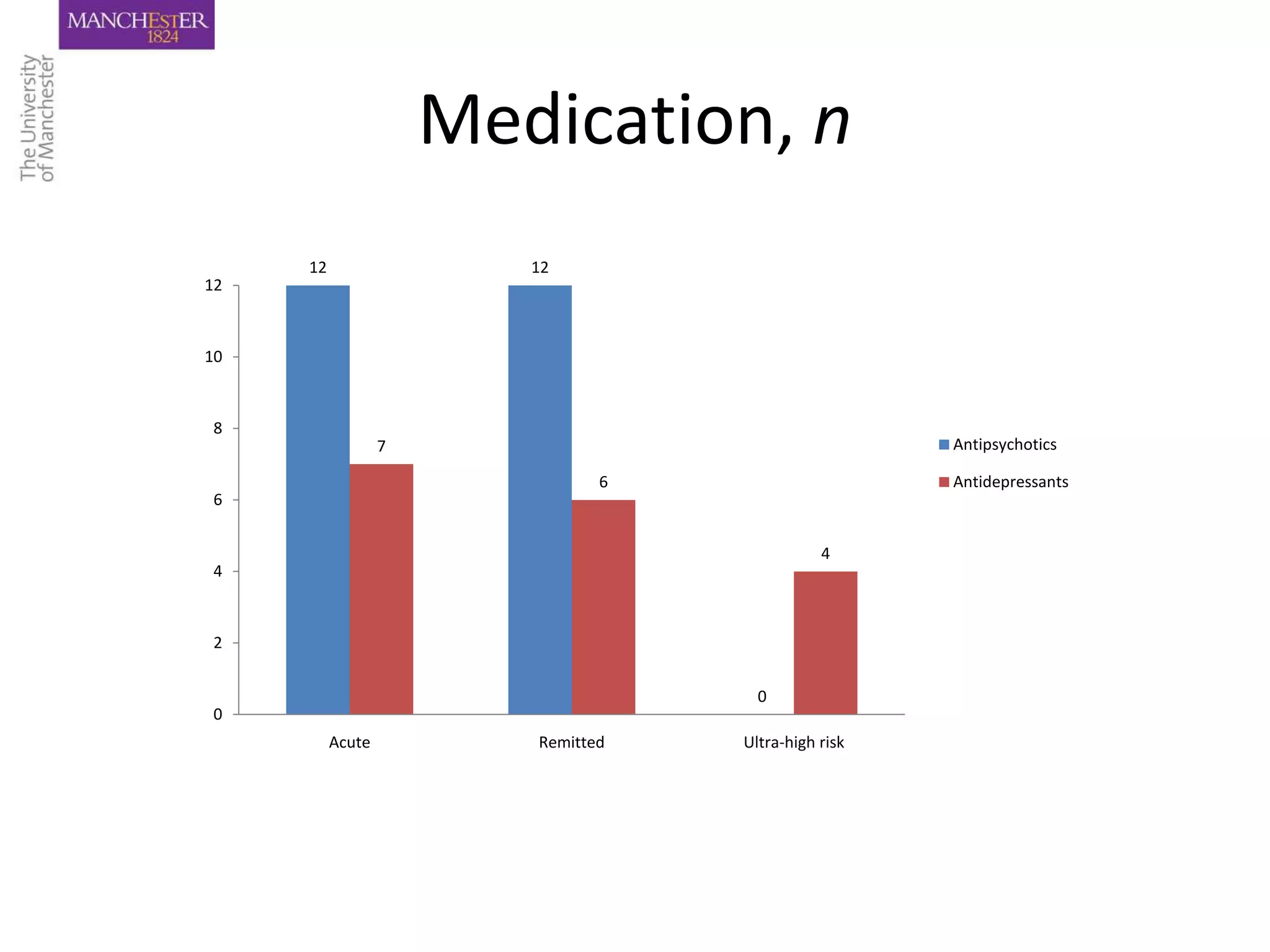
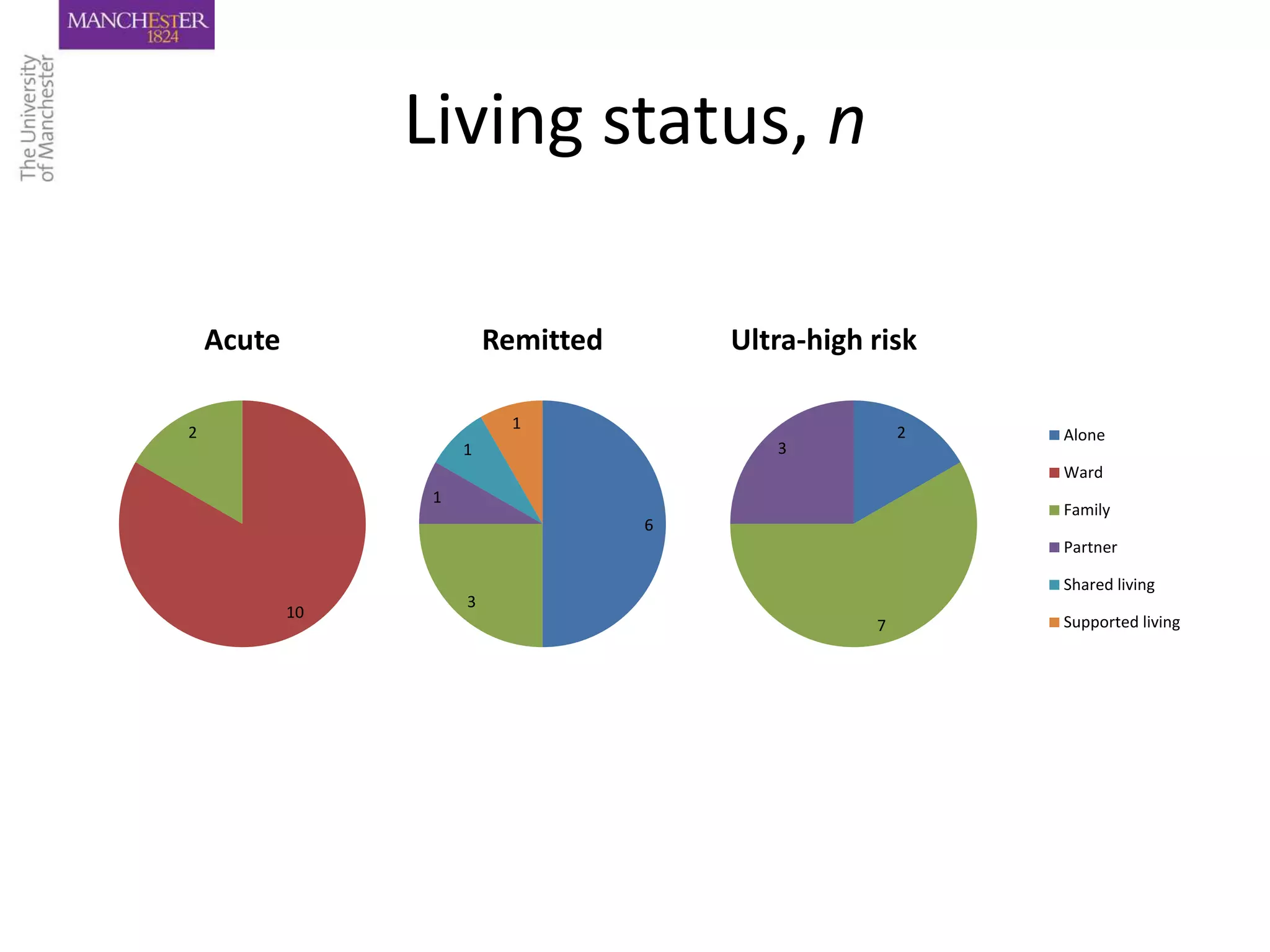
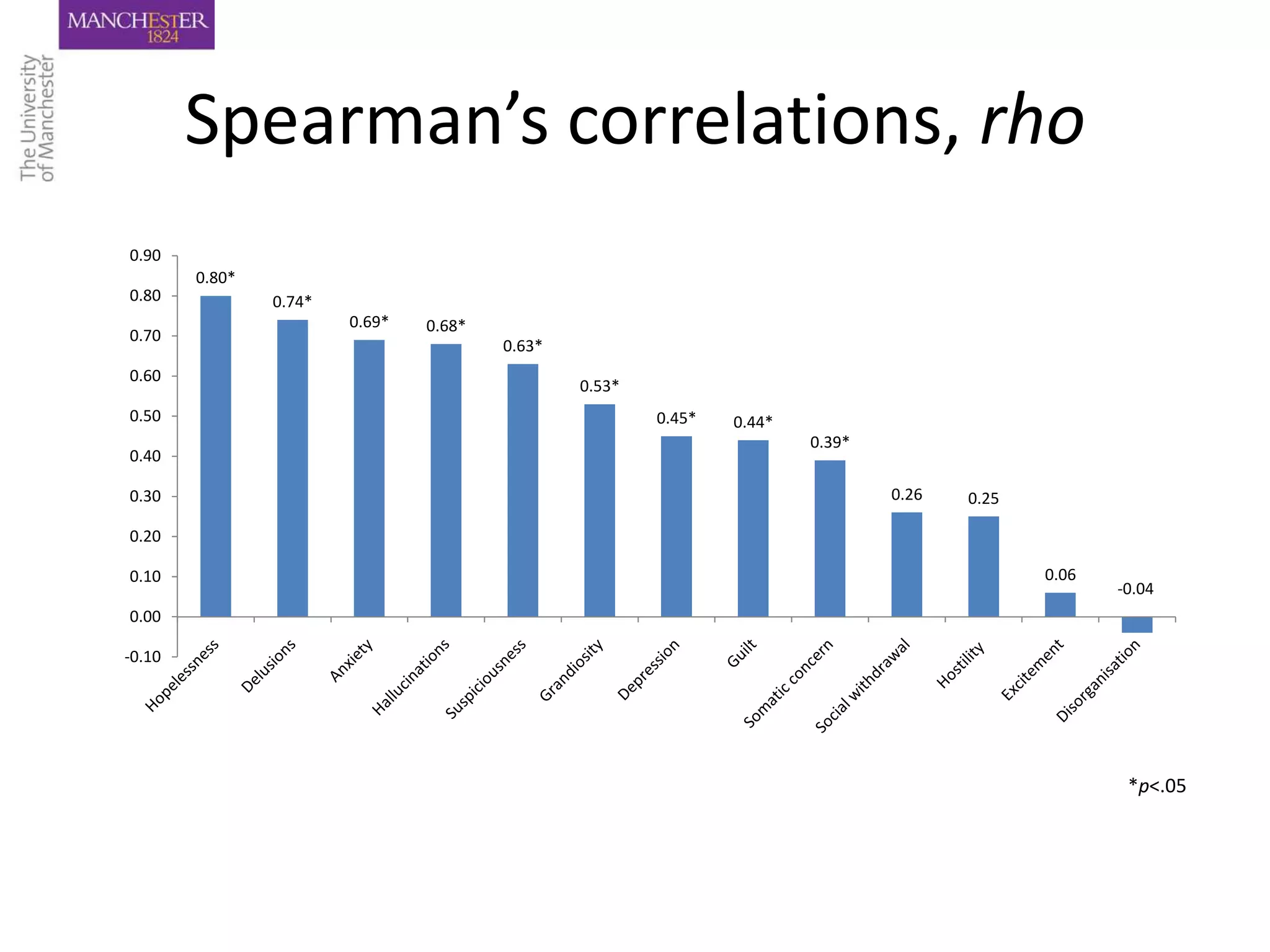
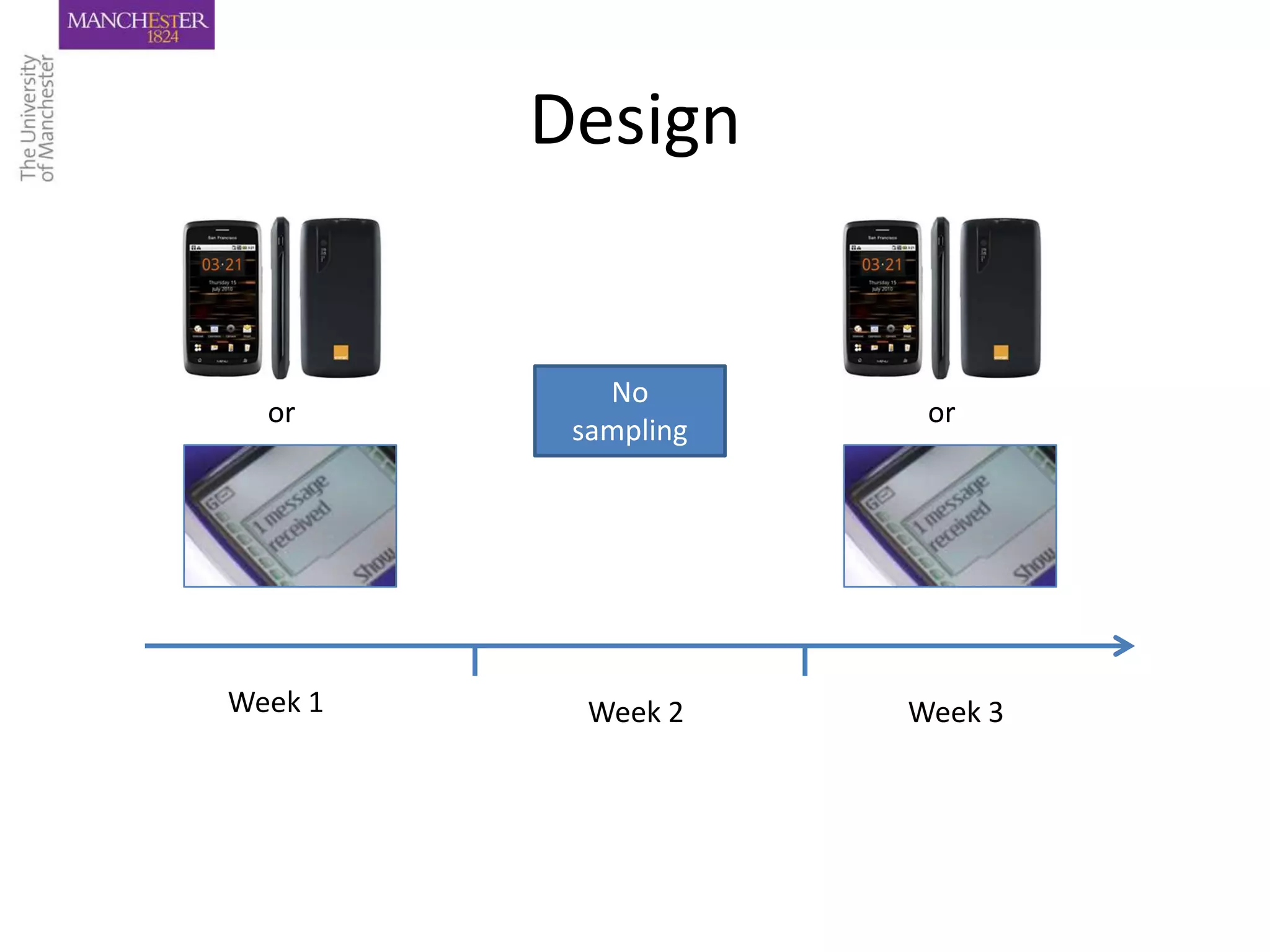
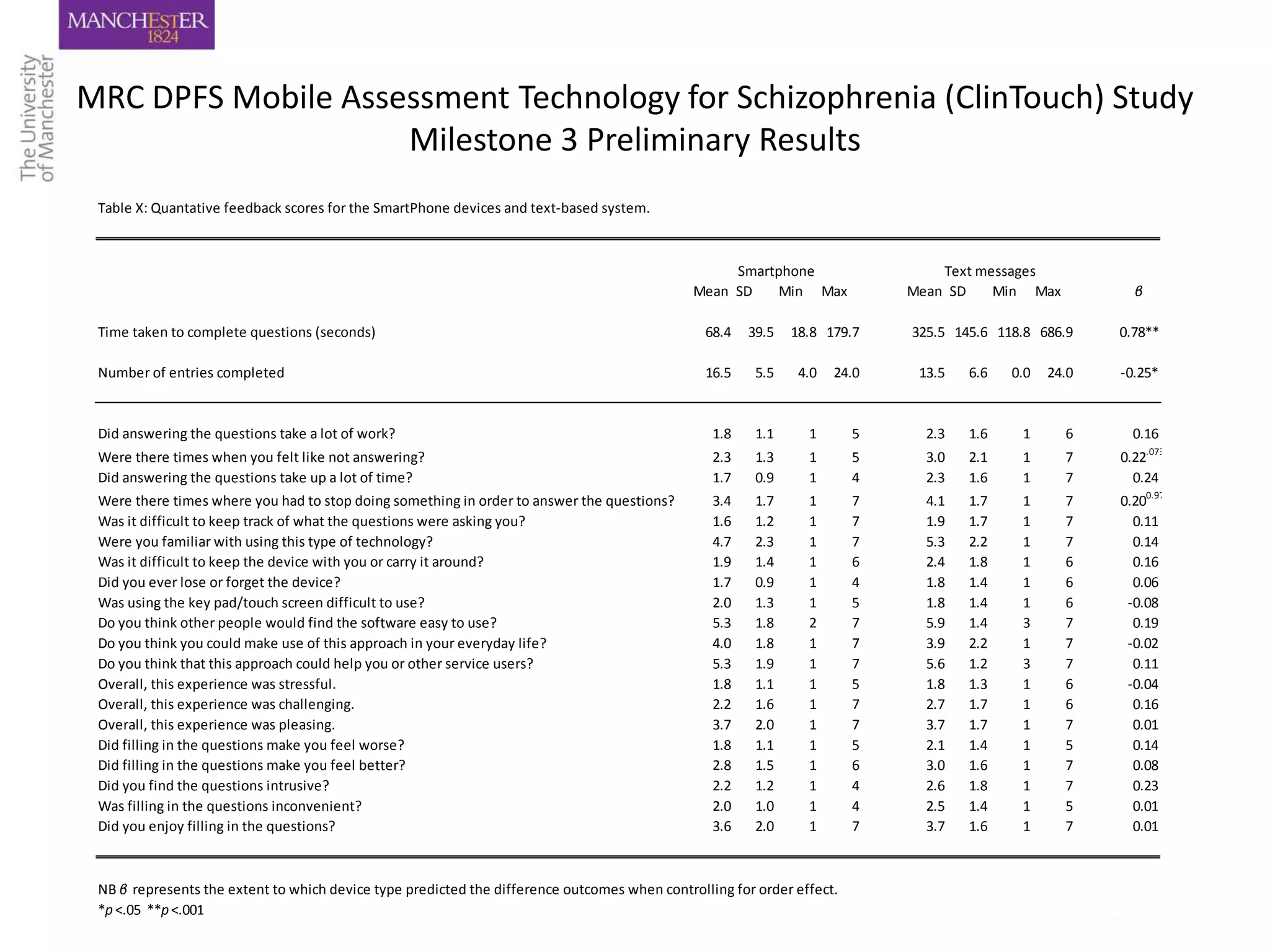
This document discusses the development and testing of a mobile assessment technology for psychosis. It describes how momentary assessment using mobile phones can provide detailed, real-time data on symptoms in everyday settings. A two-phase study was conducted to validate items on the mobile app against clinical scales and examine compliance. The results found high compliance rates and that momentary assessment is a feasible method for monitoring symptoms of psychosis.






![Quote
‘This is like quantitative stuff isn’t it? So as long
as it was balanced with interviews, however
often that person needs them then yeah [it
would be useful], but I wouldn’t give all the
power to the robots just yet. I think it would be
useful, but not to put all of our eggs in one
basket’](https://image.slidesharecdn.com/mhealthintrohim-120726035455-phpapp021-130304104701-phpapp02/75/Mhealthintrohim-120726035455-phpapp02-1-39-2048.jpg)