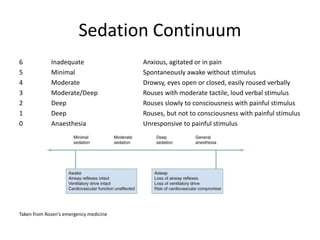
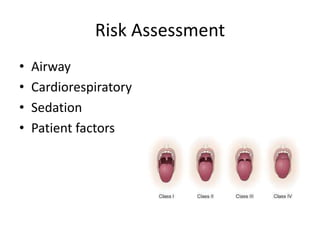
This document discusses procedural sedation, including definitions, safety considerations, and guidelines. It defines procedural sedation as inducing tolerance of uncomfortable medical procedures while maintaining cardiorespiratory function. Key risks include airway compromise and depression of breathing and circulation. Safety requires assessing risk, adequate staffing and monitoring, and managing deterioration. Guidelines recommend training, consent, monitoring including pulse oximetry and capnography, and recovery protocols. Propofol, ketamine, and midazolam are common sedative agents while fentanyl and ketamine provide analgesia.