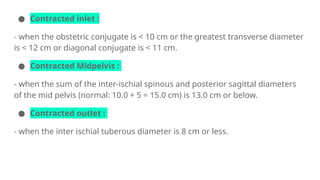
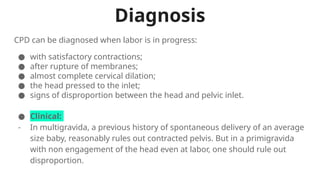
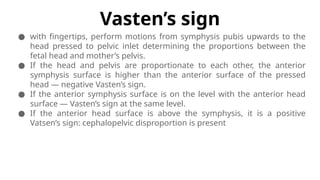
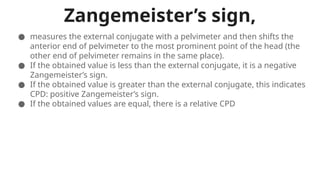
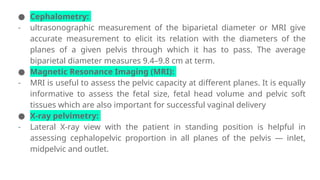
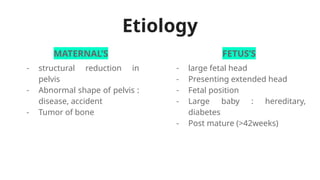
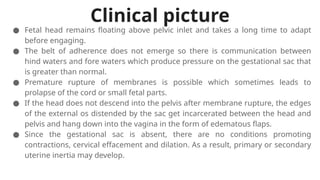
Clinically contracted pelvis, or cephalopelvic disproportion (CPD), occurs when pelvic dimensions prevent fetal passage, diagnosed through various clinical signs and examinations. Its etiology includes maternal and fetal factors, and can lead to complications such as prolonged labor and fetal distress. Treatment options involve trial labor, with potential outcomes including spontaneous delivery, assisted delivery, or cesarean section, particularly if significant disproportion is present.