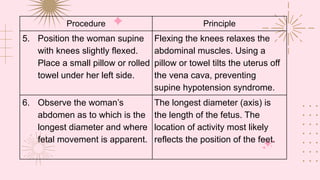
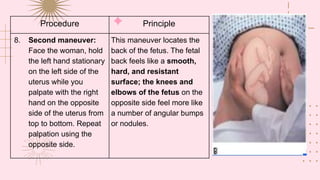
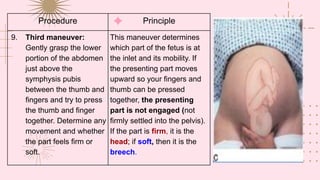
Leopold's Maneuver is used to determine the position and orientation of the fetus through abdominal palpation. It involves 4 specific palpation techniques performed by a healthcare provider: 1) palpating the fundus to determine if the fetal head or breech is present, 2) locating the fetal back by palpating opposite sides of the uterus, 3) determining if the presenting part is engaged by pressing on the lower abdomen, and 4) assessing fetal attitude and position by placing fingers along the uterine wall. The results of Leopold's Maneuver can indicate whether the fetus is positioned correctly for birth.