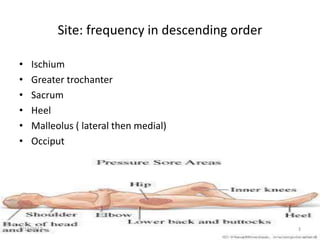
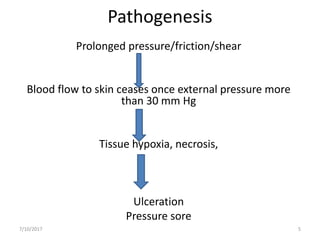
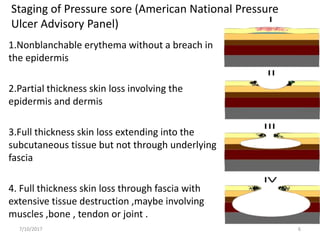
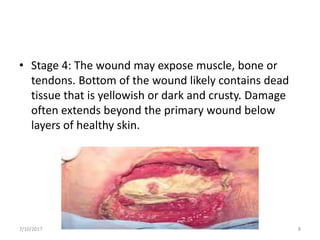
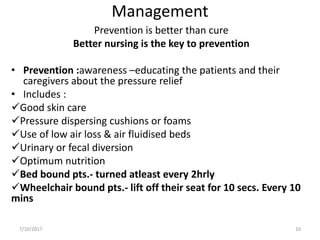
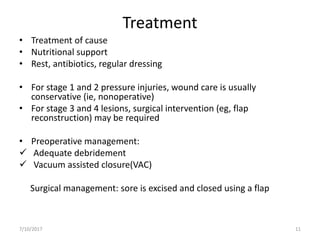
Pressure sores, also known as bedsores or decubitus ulcers, are areas of damaged skin and underlying tissue that develop when prolonged pressure is placed on certain areas of the body. They are most common on the ischium, greater trochanter, sacrum, heel, and malleolus. Risk factors include malnutrition, diabetes, peripheral vascular disease, altered mental status, and smoking. Pressure sores develop when prolonged pressure cuts off blood flow to the skin for over 30 minutes, causing tissue hypoxia and necrosis. They are staged from 1 to 4 based on severity of skin and tissue damage. Prevention through proper nutrition, skin care, pressure-relieving devices and frequent repositioning is important to