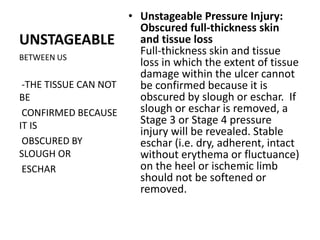
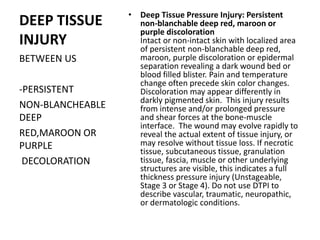
The document provides a detailed overview of skin and wound care, covering key terms, types of wounds, and specific care requirements, particularly for older adults and children. It emphasizes the importance of prevention strategies to avoid pressure ulcers, including regular patient repositioning and proper skin hygiene. Additionally, the document outlines the stages of pressure injuries and the necessary steps for caring for and documenting these wounds.