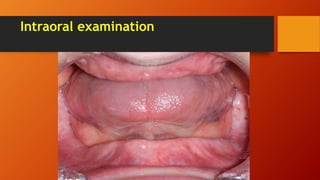
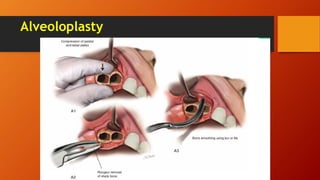
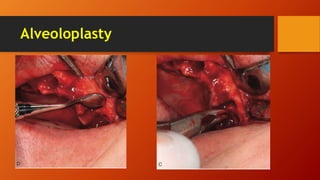
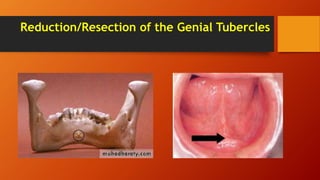
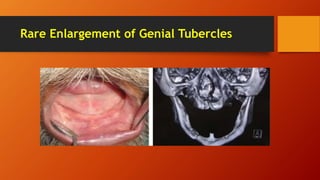
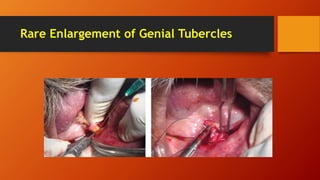
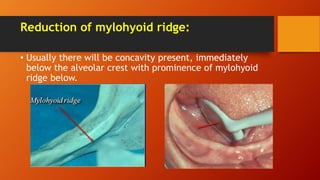
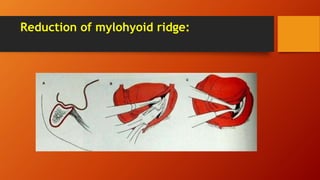
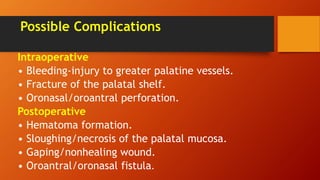
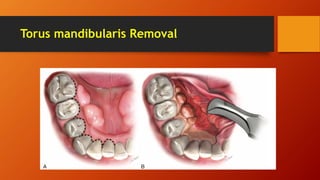
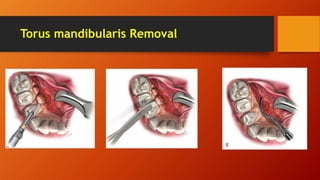
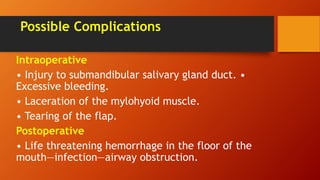
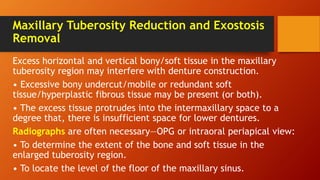
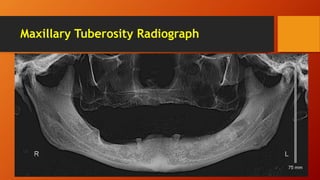
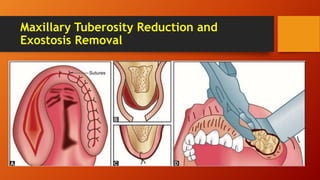
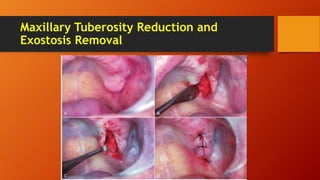
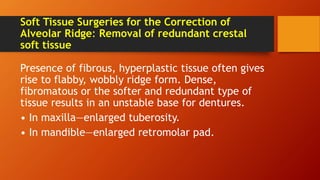
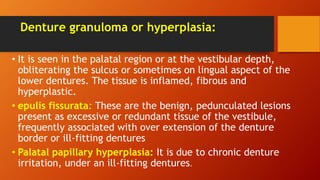
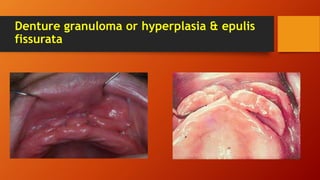
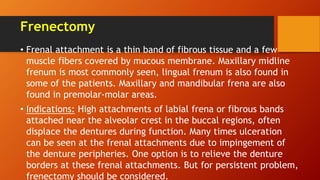
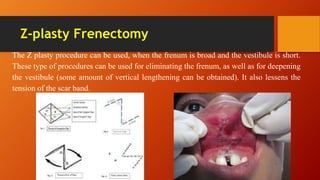
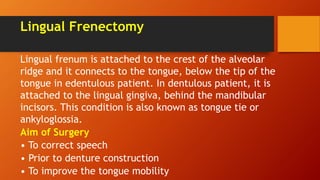
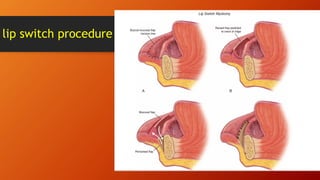
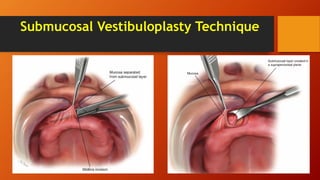
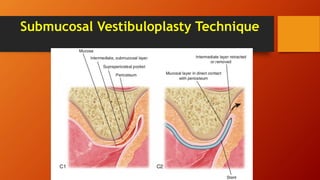
This document provides information on preprosthetic surgery procedures. It discusses the causes of edentulous bone loss over time which can negatively impact denture stability and retention. It describes various surgical techniques like alveoloplasty to recontour alveolar ridges, tori removal, frenectomy and vestibuloplasty to deepen vestibular sulci. The aim of these procedures is to provide adequate bony and soft tissue support for removable dentures. It explains how to examine patients, evaluate radiographs and plan different intraoral surgeries like genial tubercle reduction, mylohyoid ridge reduction and maxillary tuberosity reduction. Potential complications of these surgeries are also summarized.