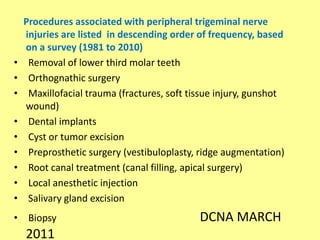
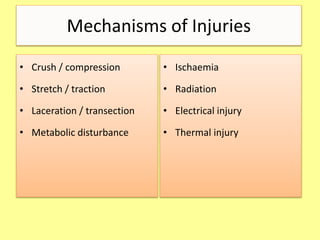
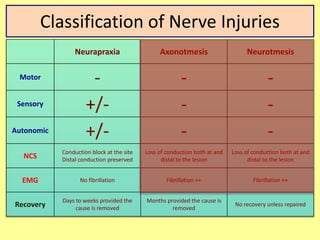
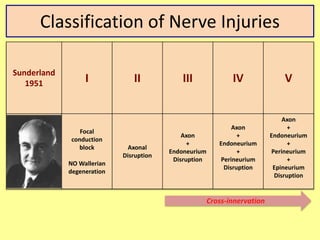
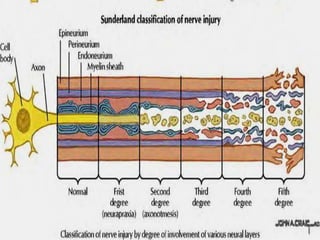
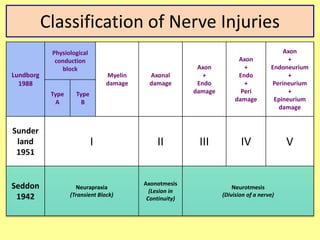
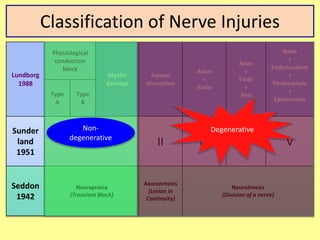
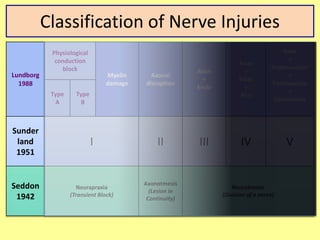
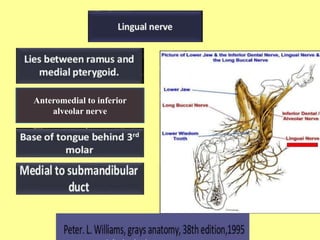
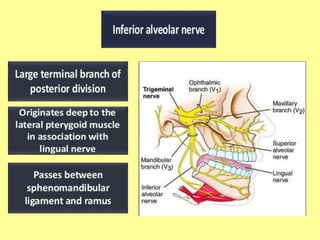
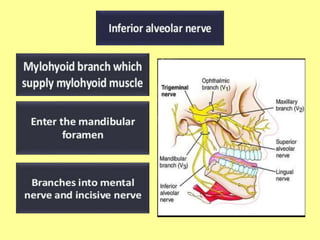
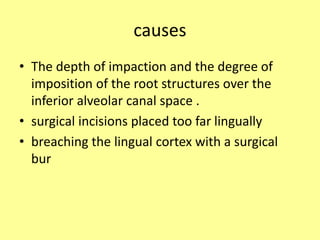
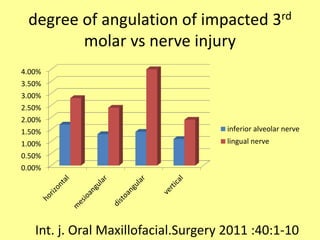
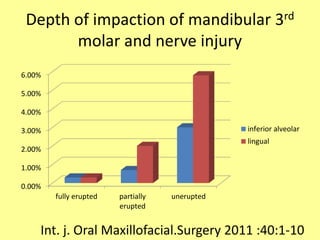
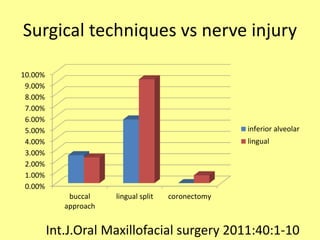
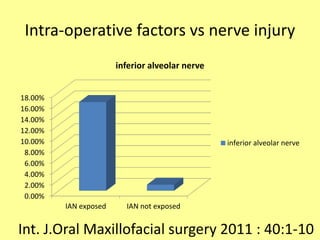
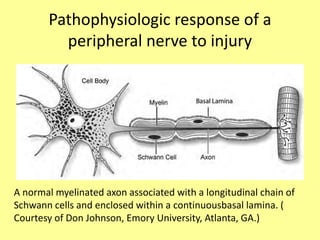
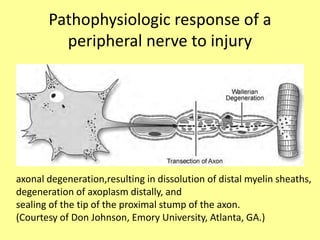
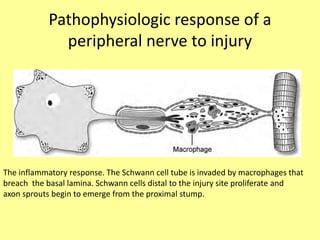
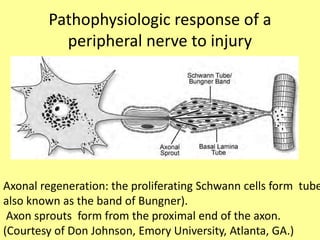
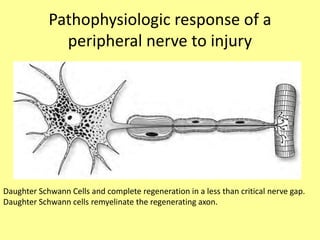
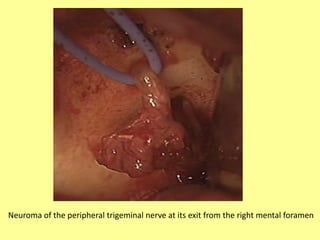
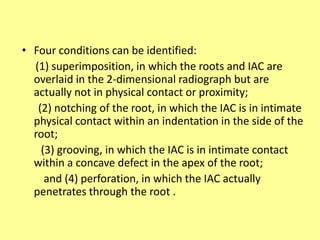
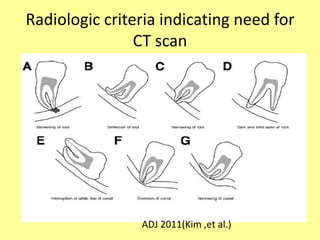
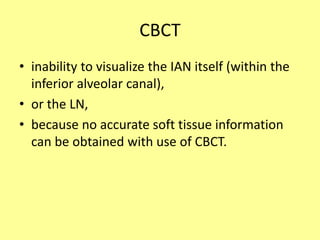
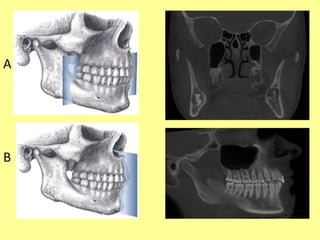
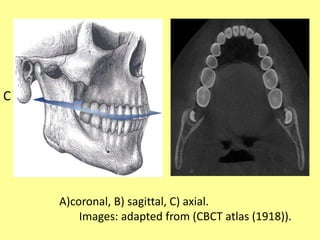
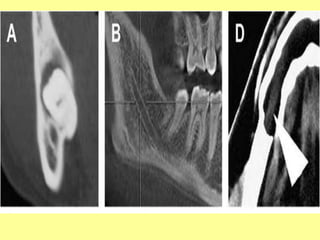
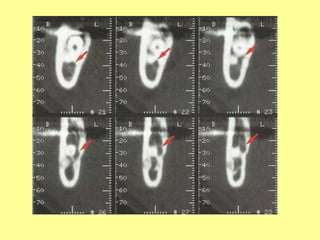
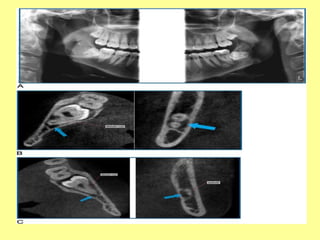
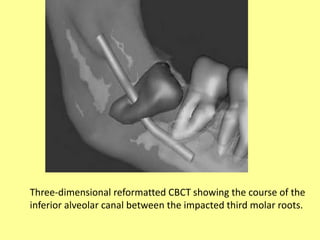
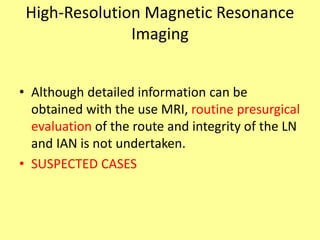
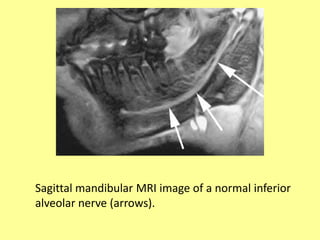
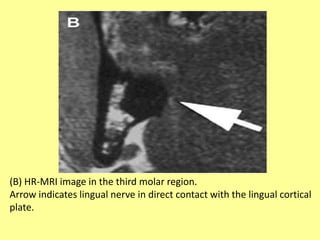
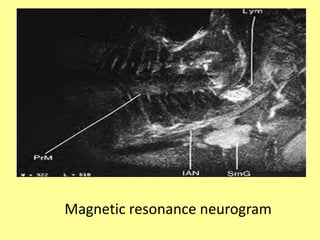
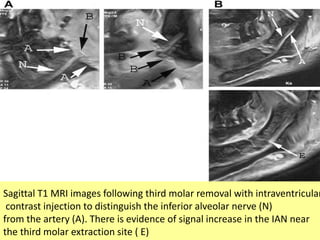
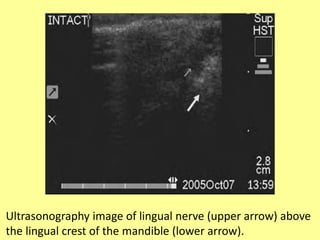
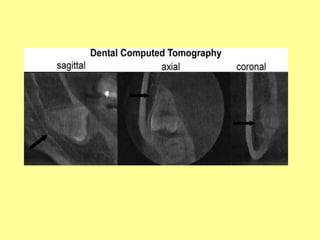
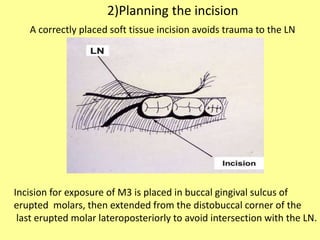
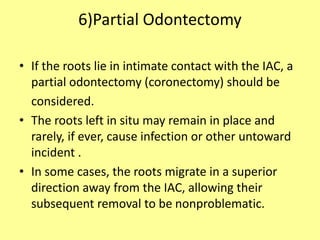
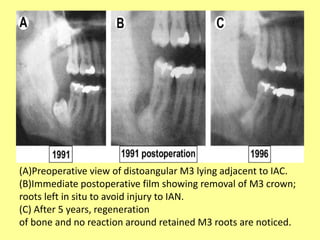
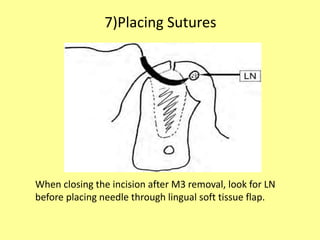
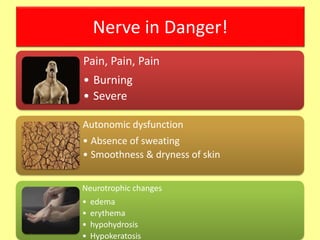
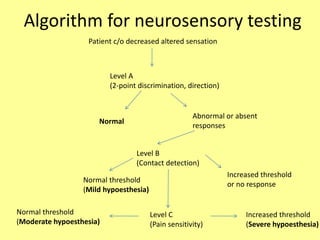
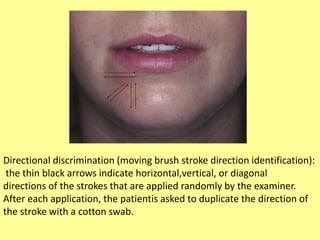
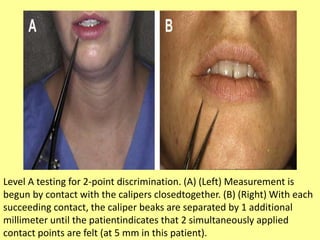
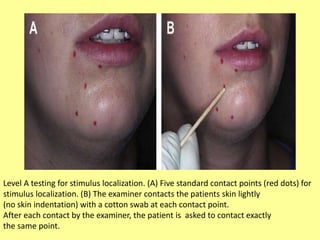
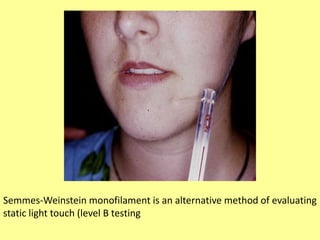
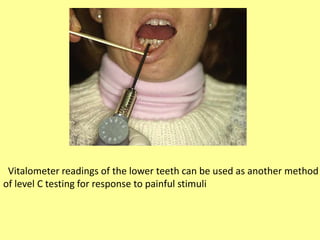
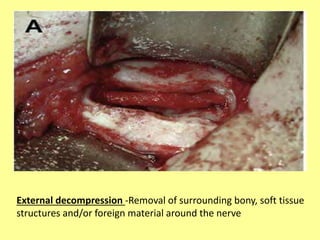
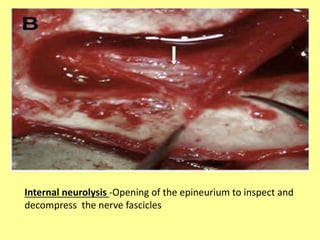
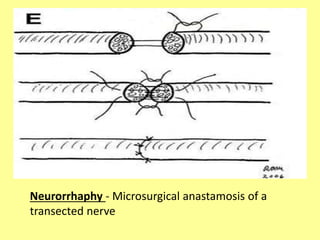
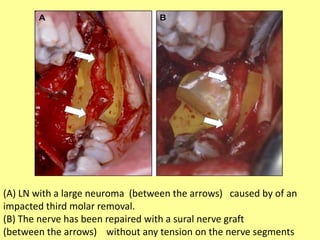
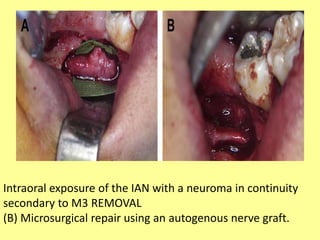
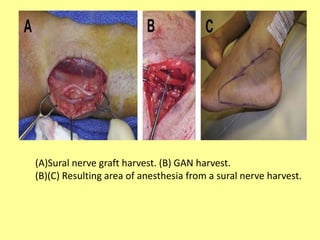
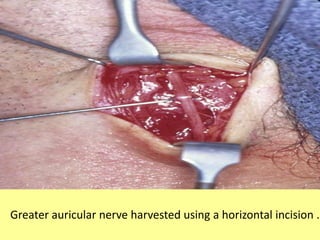
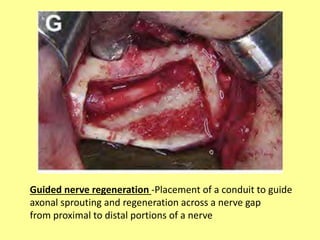
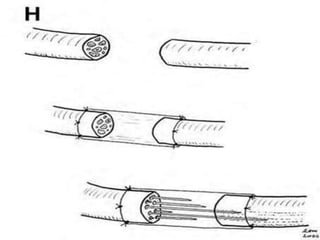
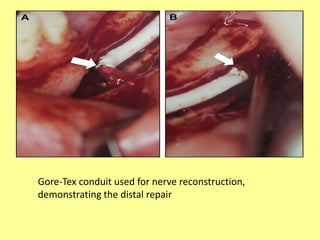
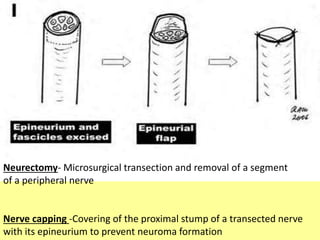
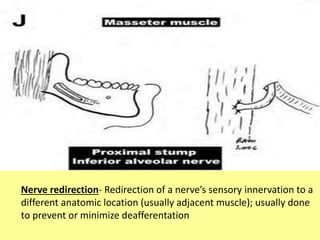
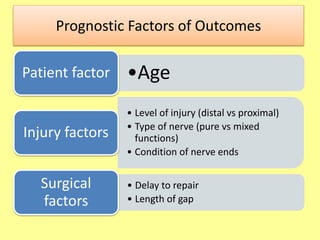
This document discusses nerve injuries that can occur during mandibular impaction surgeries such as the removal of lower third molar teeth. It provides classifications of nerve injuries including Seddon and Sunderland classifications. Mechanisms of nerve injuries include crush, stretch, laceration and ischemia. The document outlines techniques to prevent nerve injuries during surgery such as careful planning of incisions and use of imaging to identify nerves. It also discusses evaluating and managing nerve injuries post-operatively through neurosensory testing.