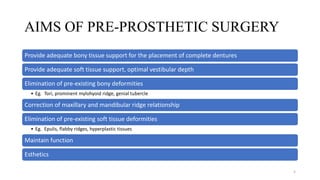
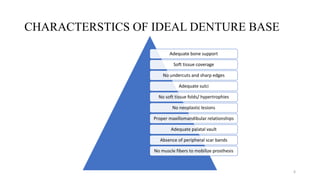
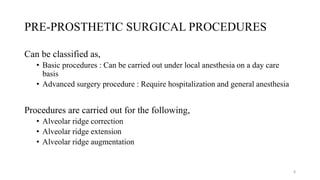
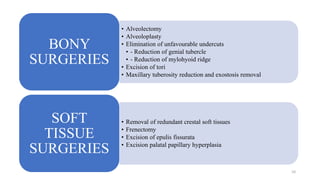
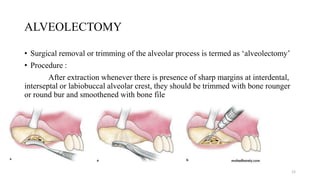
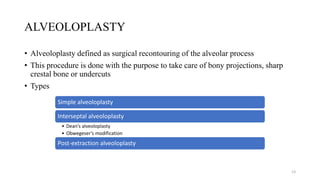
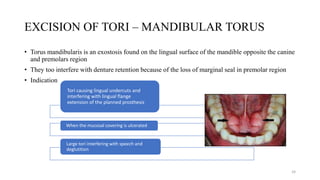
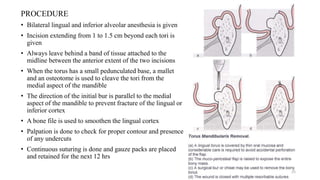
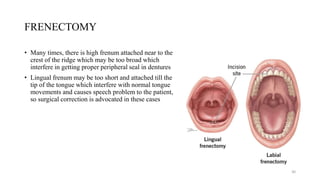
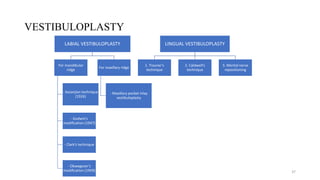
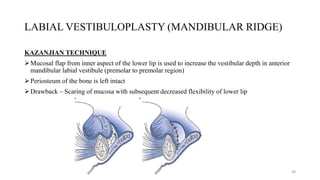
Pre-prosthetic surgery aims to improve tissue support for dentures through various surgical procedures. It involves correcting hard and soft tissue deficiencies through alveolectomy, alveoloplasty, torus removal and frenectomy. Careful patient evaluation and treatment planning is required to determine the appropriate surgical procedures needed to eliminate anatomical hindrances and provide adequate bone and soft tissue support for a stable, functional and comfortable prosthesis. Common procedures include ridge correction and augmentation through techniques like alveolar ridge reduction, vestibuloplasty and torus excision.