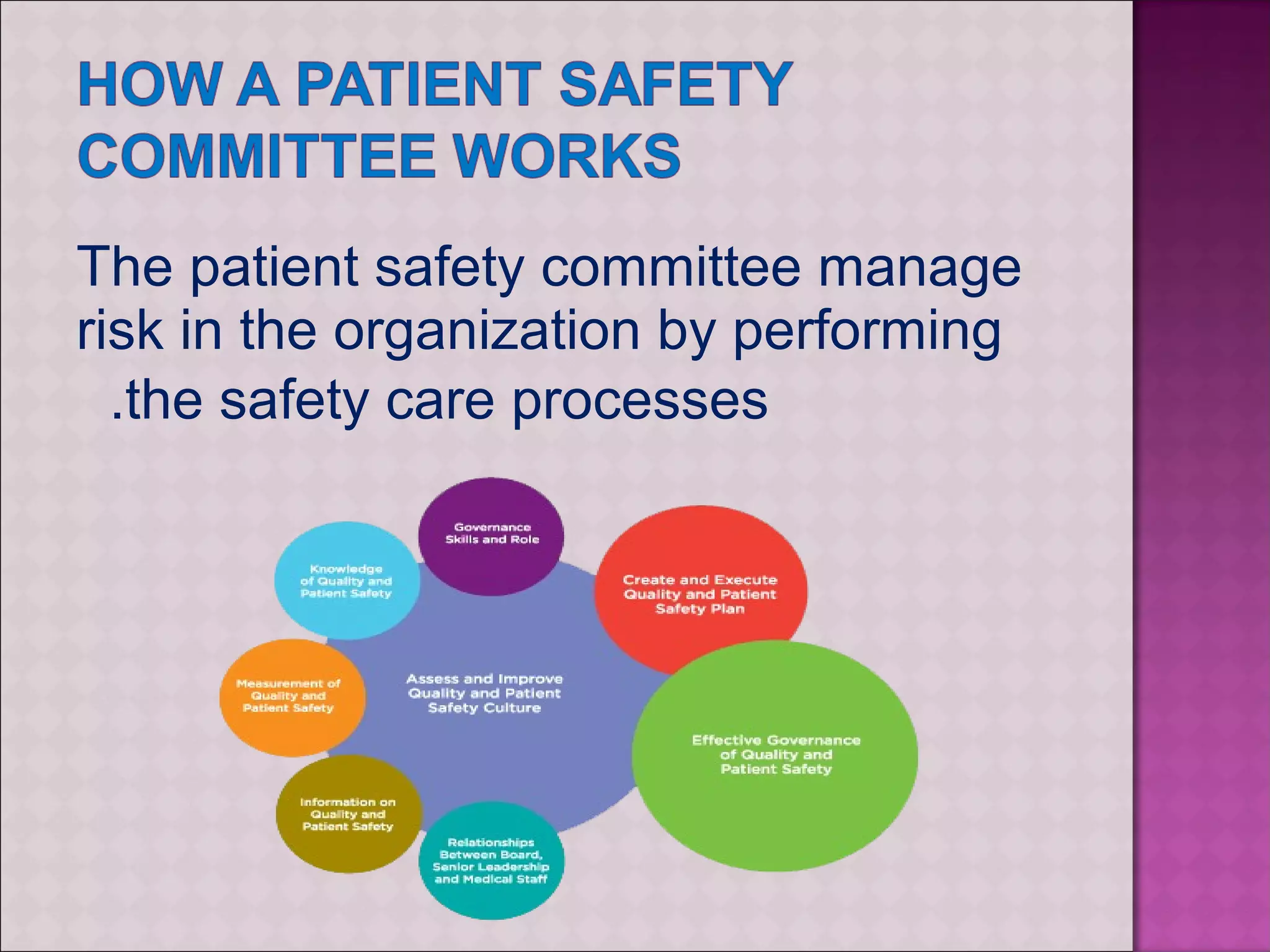
The document discusses patient safety in healthcare. It defines patient safety and identifies common medical errors. The goals are to establish a culture of safety, minimize errors, and implement standardized practices and reporting. A patient safety committee coordinates these efforts by managing risk, establishing reporting procedures, and collecting/analyzing safety data to identify root causes and implement corrective actions. The leadership role is to create an environment that recognizes safety importance and implements a patient safety program.