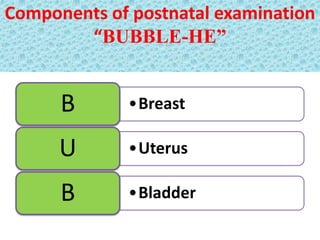
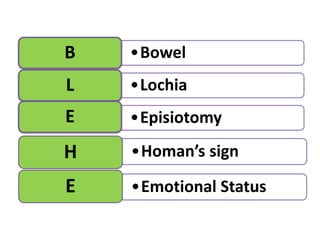
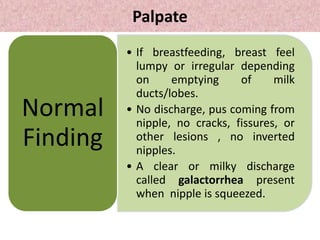
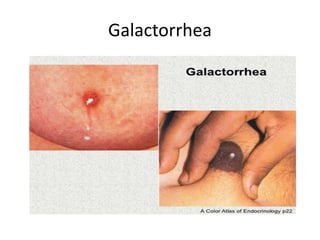
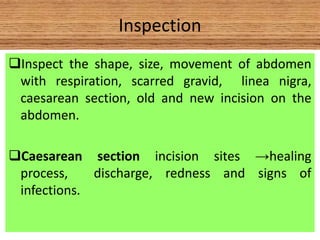
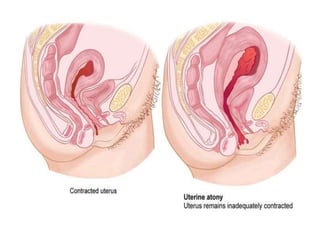
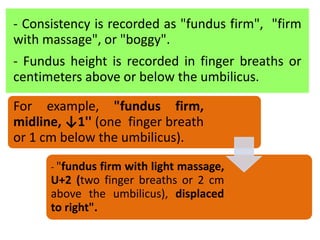
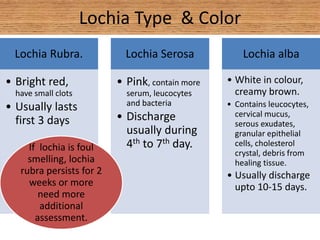
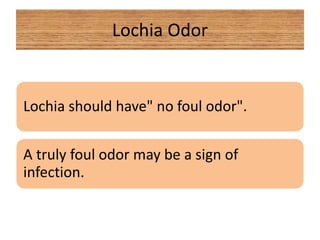
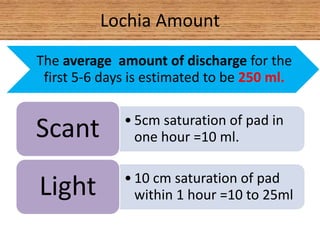
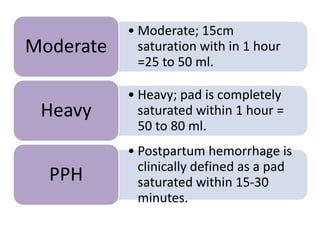
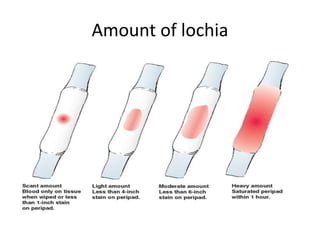
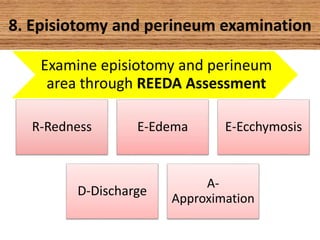
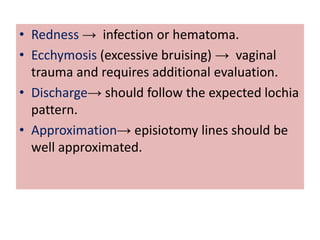
The document provides guidance on conducting a postnatal examination. The exam involves assessing vital signs, the breasts, abdomen, bladder, bowels, and lochia. Key things to check include temperature, pulse, blood pressure, skin, breasts for lumps or discharge, the uterus for size and tenderness, bladder fullness, bowel sounds, and character of lochia including color, odor, and amount. The exam aims to monitor the health of the mother and newborn and identify any issues requiring further care.