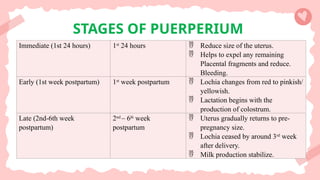
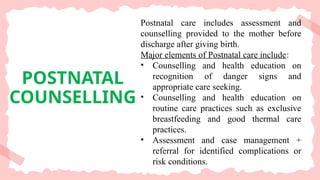
Postnatal period begins immediately after birth of baby and placenta is delivered and lasts up to 6 wks. Most of complications, such as postpartum hemorrhage, sepsis, uterine prolapse, amniotic fluid embolism and eclampsia which may lead to maternal mortality, occur during this period.
As per WHO's document on 'recommendations on maternal and newborn care for a positive postnatal experience' published in 2022 up to 30% of maternal deaths occur in postnatal period. The 4th stage of labor is the 1st hour of postnatal period and is very crucial for mother and infant.
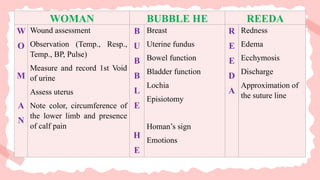
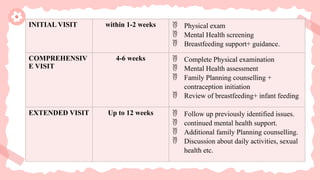
Postnatal care is special care offered to a woman and her infant during the postnatal period. It includes routine and specific clinical examination and observation of the mother and baby, routine infant screening to detect any abnormalities.
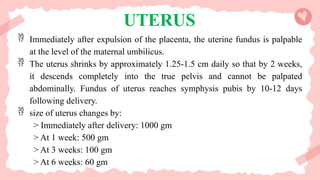
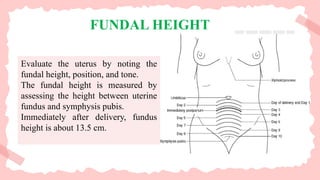
puerperium can be defined as the period after childbirth till 6 weeks postpartum, in which pelvic organs return to the pre-pregnancy state both anatomically and physiologically.