The document defines erectile dysfunction and discusses its pathophysiology, epidemiology, classification, diagnostic evaluation, and treatment options. Some key points:
- Erectile dysfunction is defined as the inability to attain/maintain an erection for satisfactory sexual performance for 3 months.
- Prevalence increases with age, ranging from 6-64% depending on age subgroups according to studies.
- Causes can be organic, relational, psychological or a mix (primary or secondary).
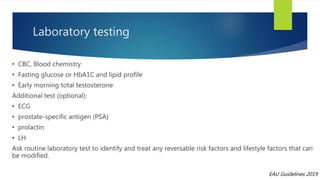
- Evaluation involves medical history, physical exam, questionnaires, and optional tests to identify reversible factors.
- Treatment progresses from lifestyle changes, to oral medications, injections, and finally implants if other options fail.