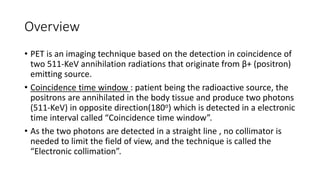
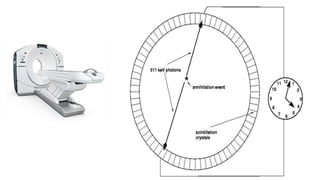
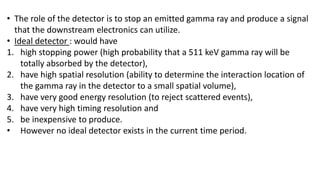
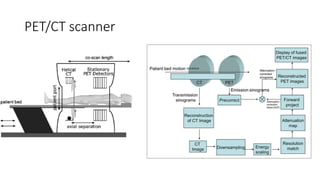
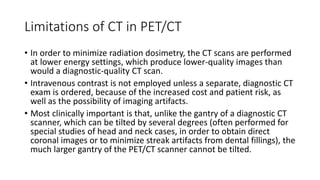
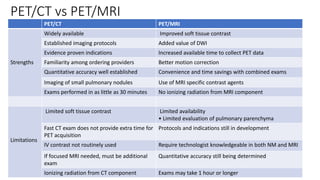
Positron Emission Tomography (PET) is a nuclear imaging technique that detects pairs of gamma rays emitted by a positron-emitting radiotracer to produce three-dimensional images of functional processes in the body. PET scans are often combined with computed tomography (CT) to provide both functional and anatomic information. PET/CT has advantages over PET alone in improving diagnostic accuracy, decreasing scan time, and better localizing areas of abnormal activity. Limitations include increased radiation exposure compared to PET and potential motion artifacts from combining the two modalities. Emerging hybrid imaging technologies include PET/MRI which provides improved soft tissue contrast compared to CT but also faces challenges from the magnetic fields interfering with standard PET detector technology.