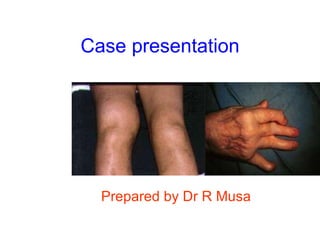
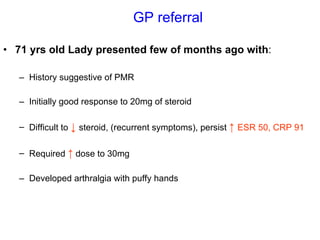
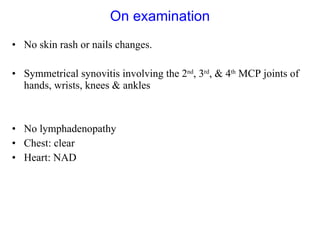
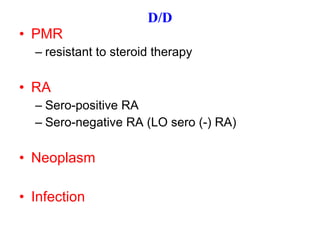
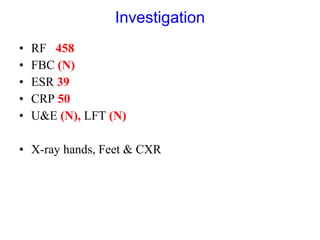
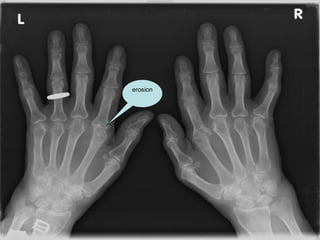
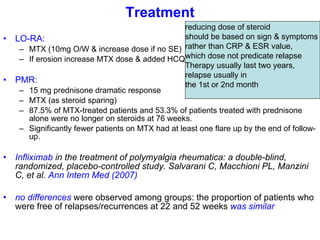
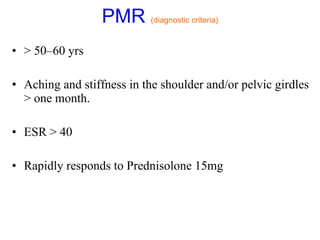
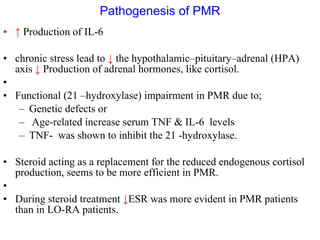
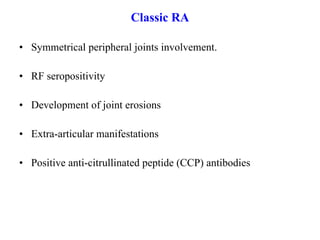
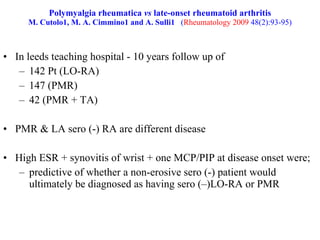
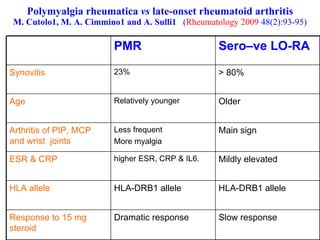
A 71-year-old woman presented with aching pain and stiffness in her arms, hands, knees and feet for several months. She responded well initially to steroid treatment but had difficulty tapering off the dose. Examination found symmetrical joint swelling. Tests showed elevated inflammatory markers. She was diagnosed with possible polymyalgia rheumatica or late-onset rheumatoid arthritis. Treatment with methotrexate and gradual steroid tapering was recommended.