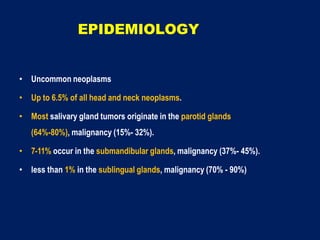
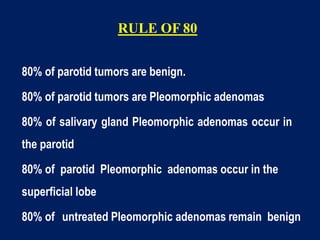
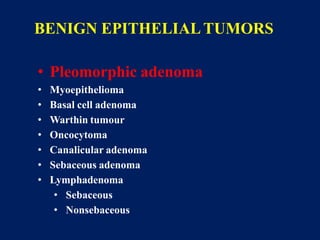
1) Salivary gland tumors are mostly benign (80%), with the majority originating in the parotid glands.
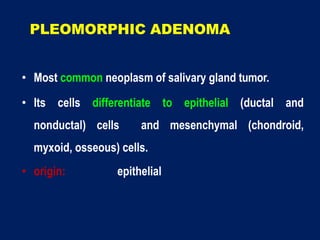
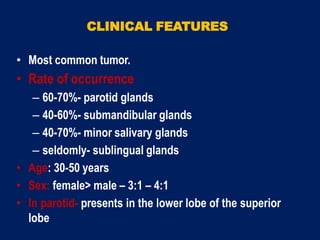
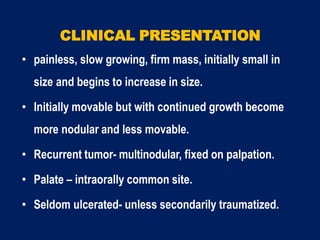
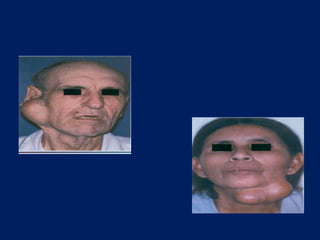
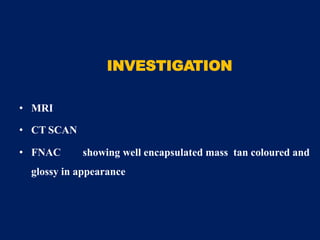
2) Pleomorphic adenoma is the most common benign tumor, representing 80% of parotid gland tumors.
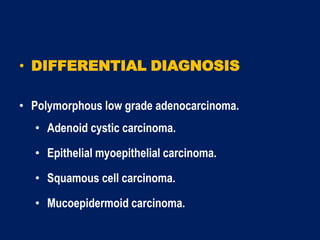
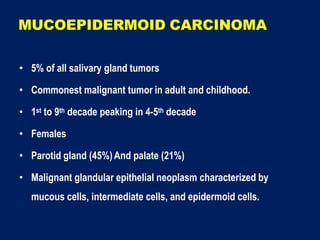
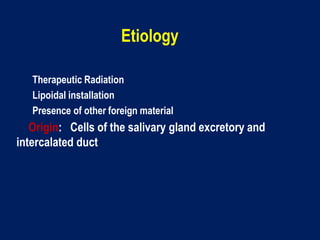
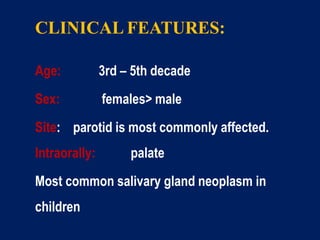
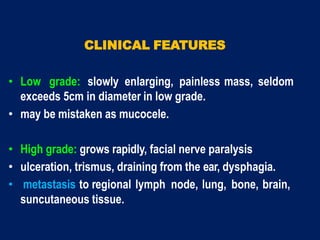
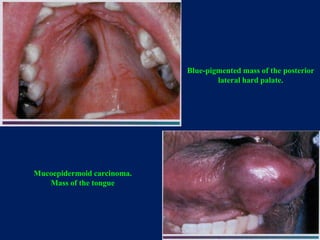
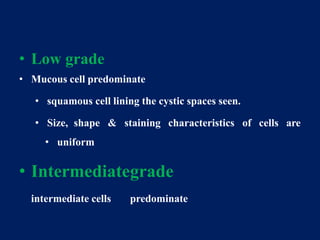
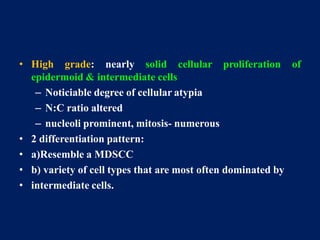
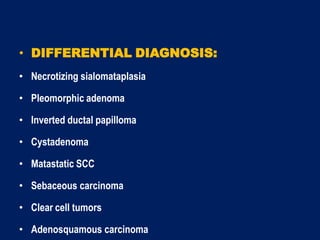
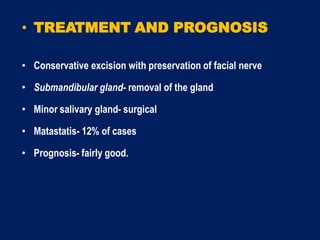
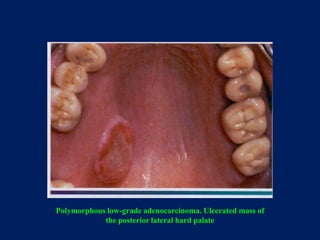
3) Mucoepidermoid carcinoma is the most common malignant salivary gland tumor in both adults and children, typically presenting as a slow-growing mass in the parotid gland or palate.