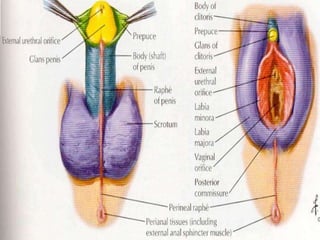
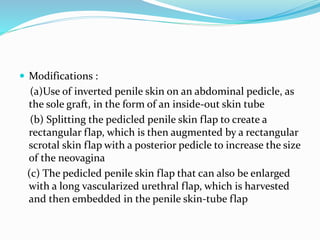
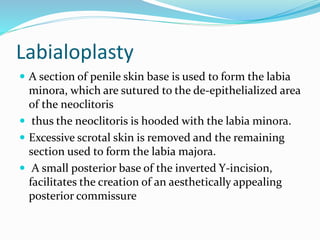
The document discusses transsexualism and various surgical techniques for vaginoplasty in male-to-female sex reassignment surgery. It defines transsexualism and lists diagnostic criteria. It then describes different surgical techniques for vaginoplasty including penile skin grafts, genital skin flaps, and nongenital skin flaps. It discusses goals of creating a functional vagina and satisfactory sexual function. It also covers related procedures like labiaplasty, clitoroplasty, and vaginopexy. The document emphasizes the importance of adequate depth, sensation, and aesthetic appearance of the neovagina for sexual satisfaction and fulfillment of patients' expectations.