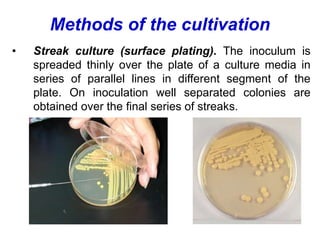
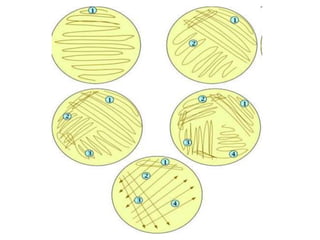
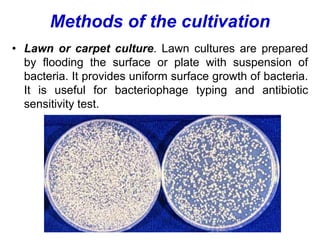
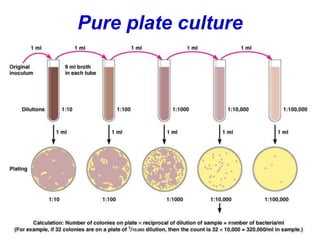
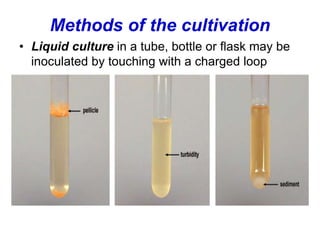
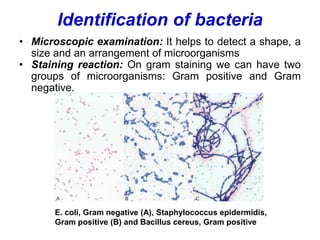
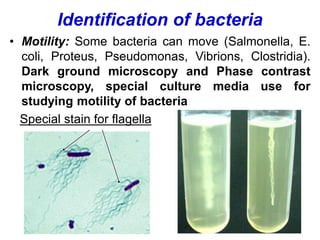
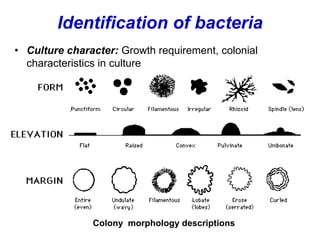
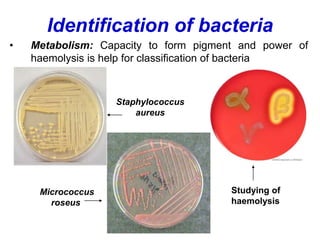
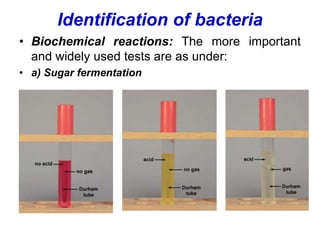
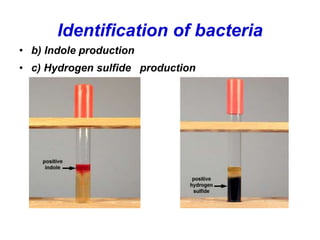
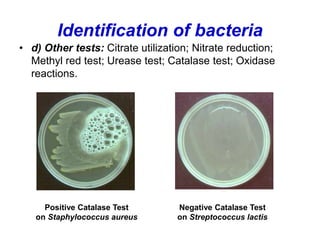
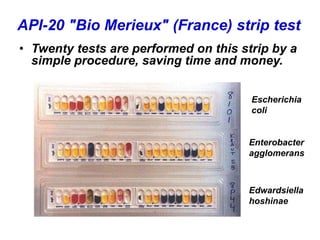
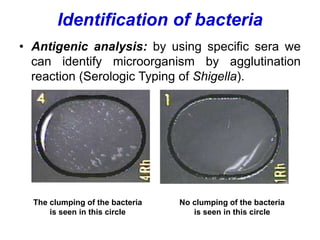
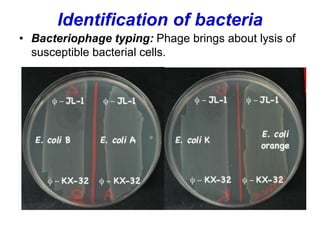
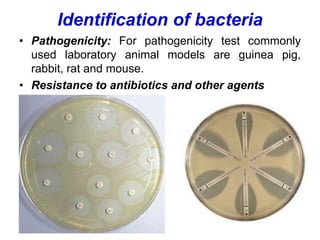
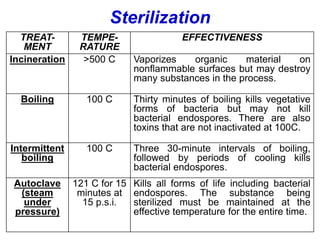
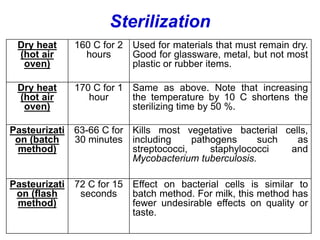
This document discusses various methods for laboratory diagnosis and cultivation of bacteria, as well as identification. It describes microscopic examination, culture methods, and tests to determine sensitivity to antibiotics. Various culture techniques are outlined, including streak, lawn, stab and liquid cultures. Identification involves examining morphology, staining reactions, motility, metabolism, biochemical reactions, antigenic analysis and pathogenicity. Bacterial metabolism and the basic requirements for culture media are also summarized. Finally, different sterilization methods like autoclaving, boiling and dry heat are compared.