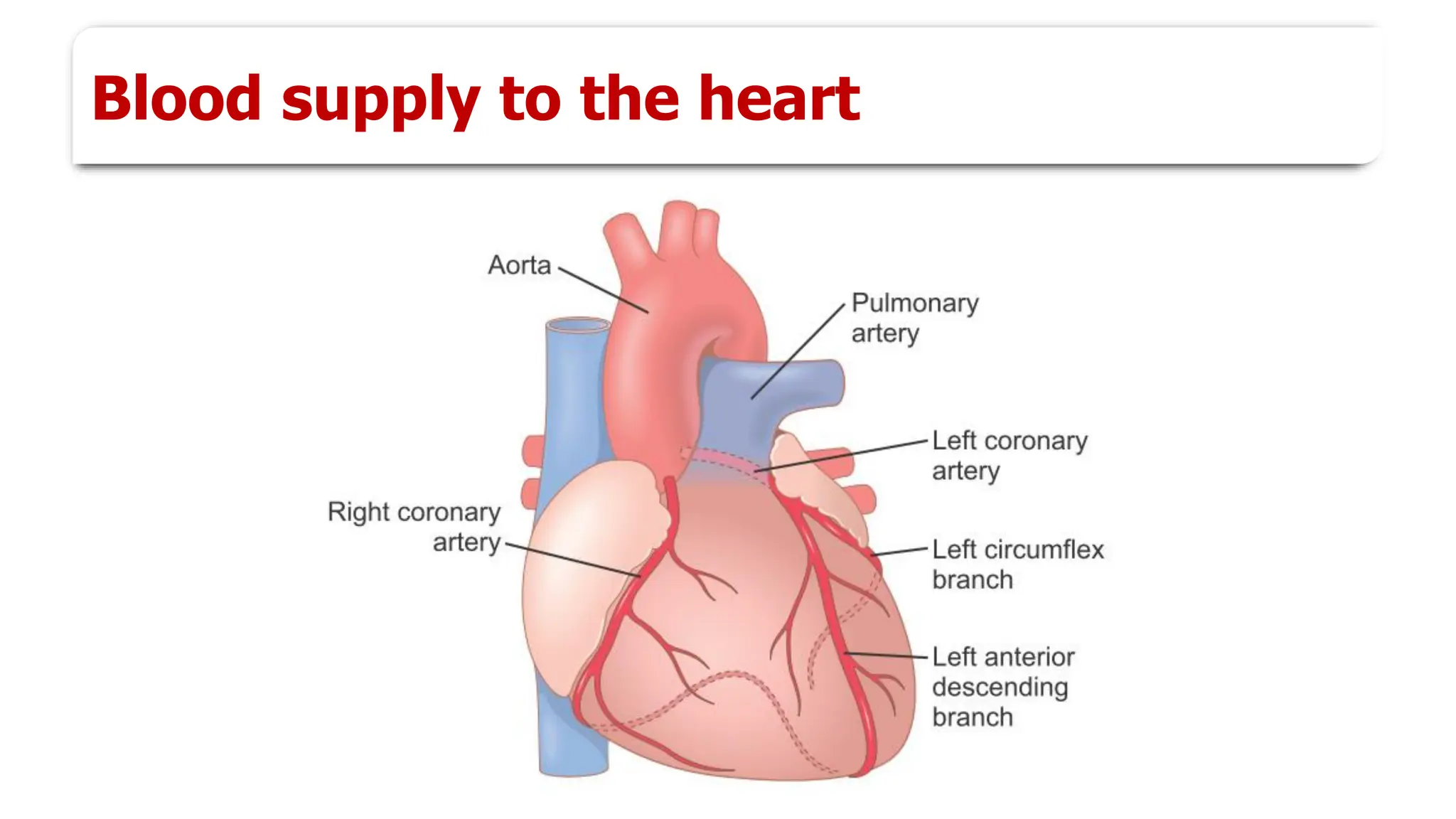
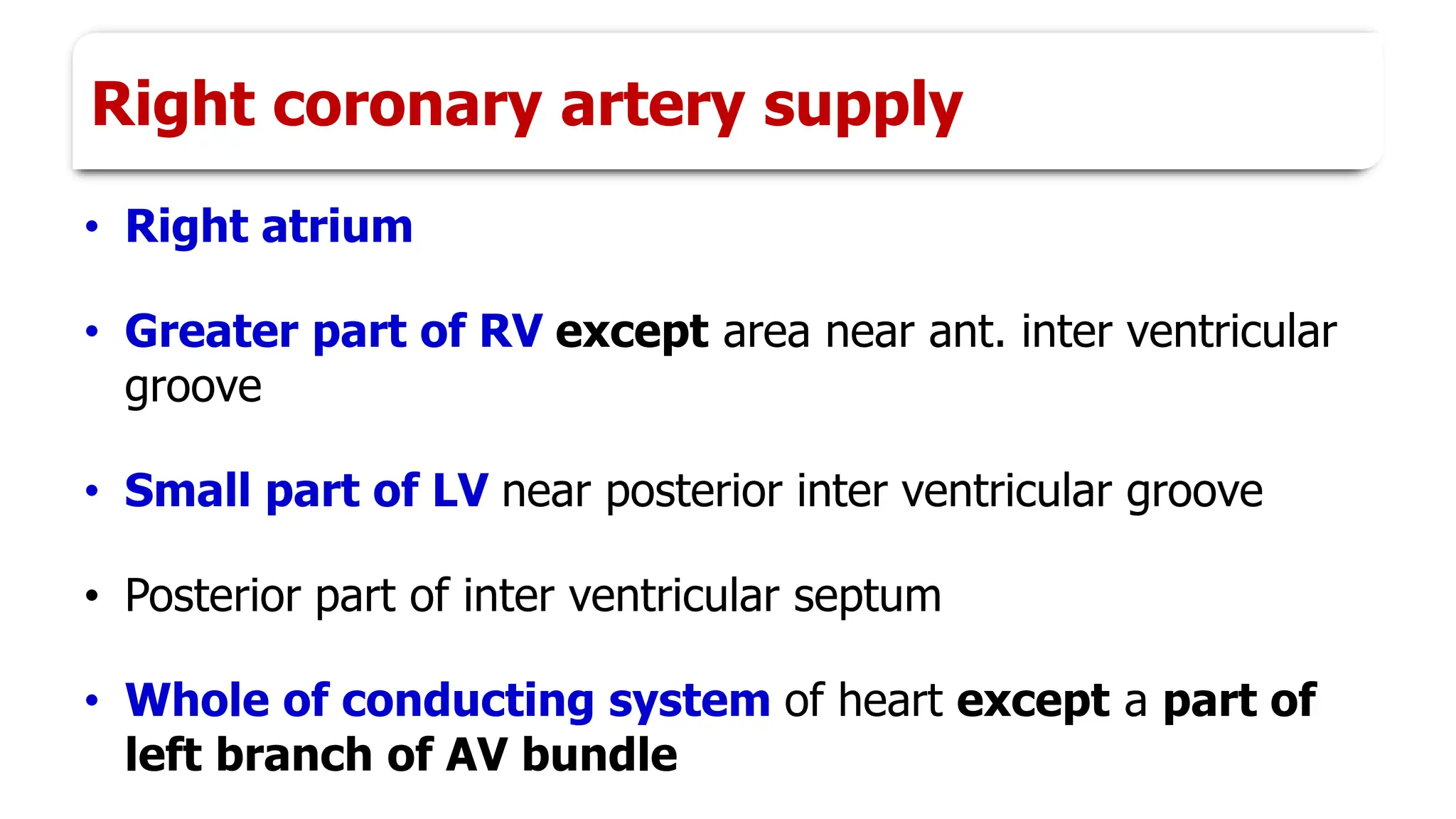
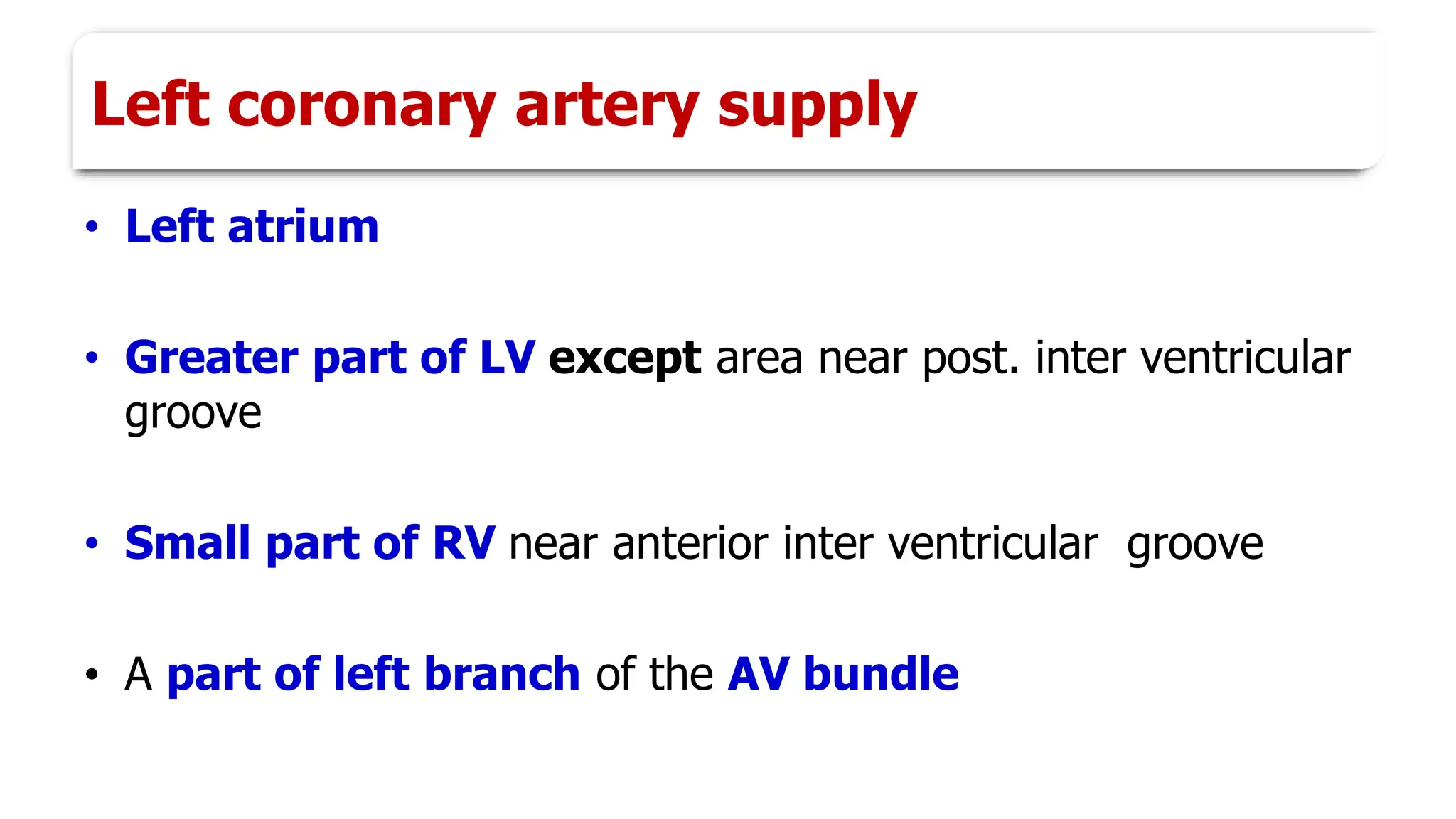
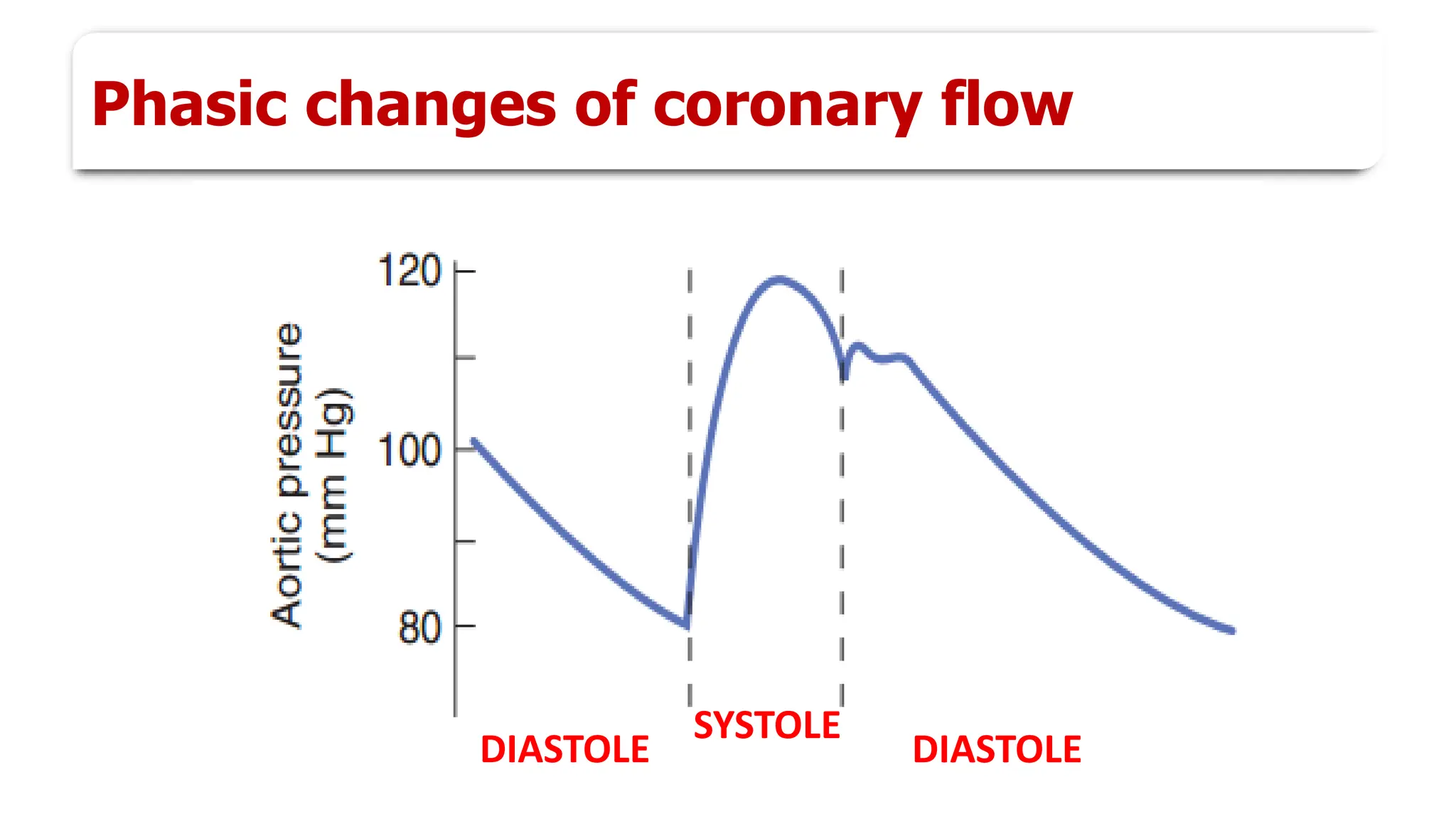
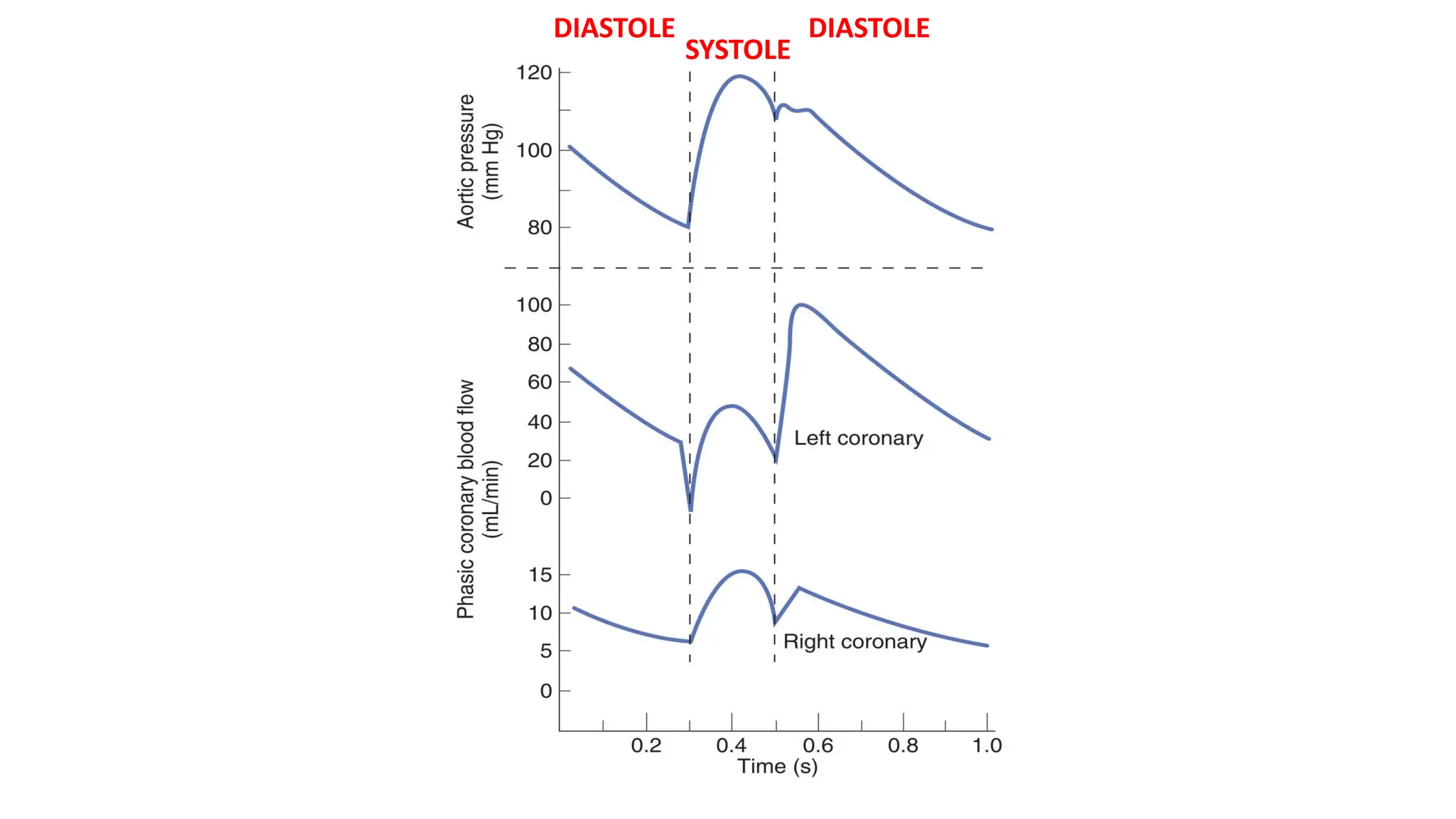
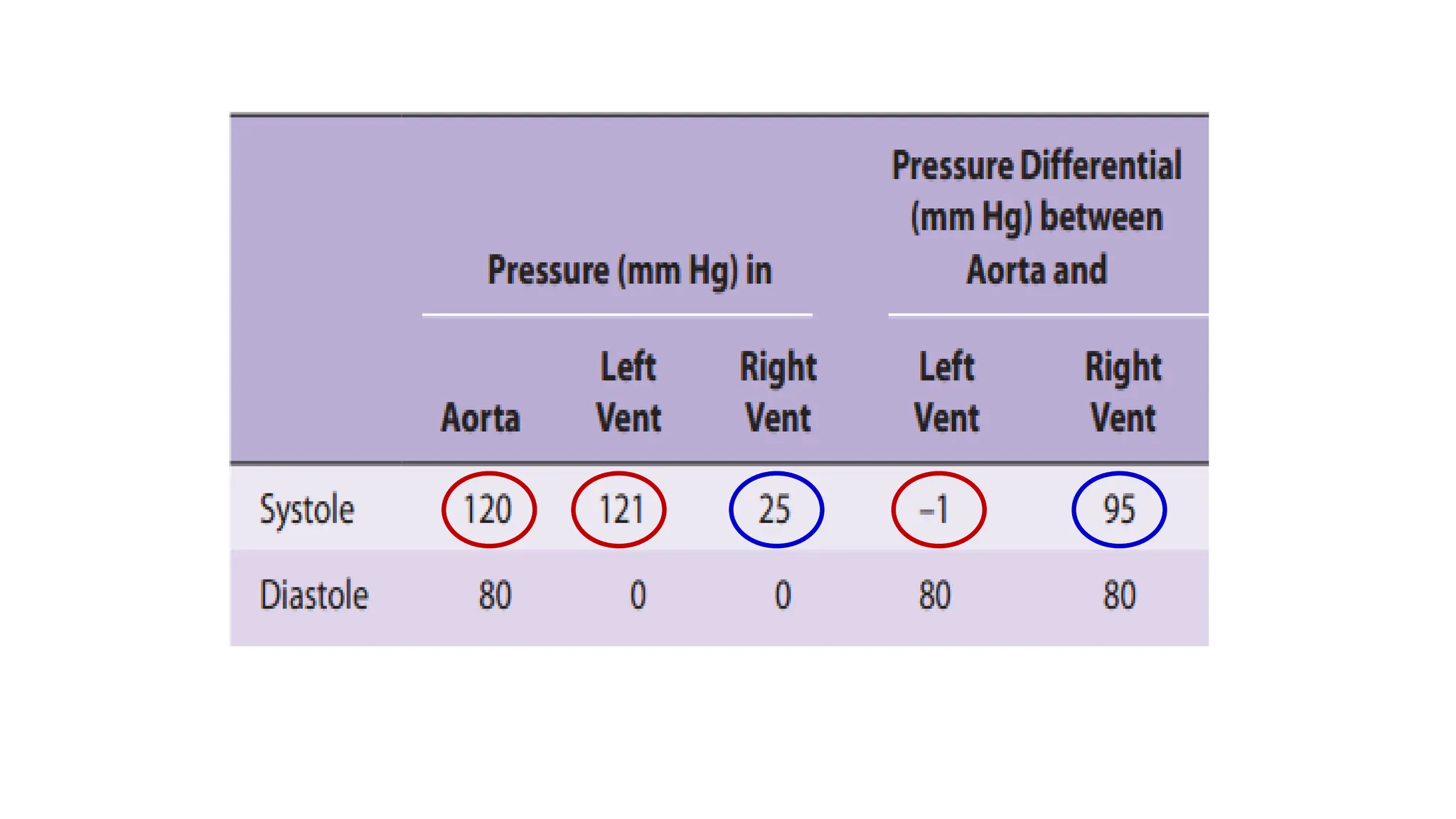
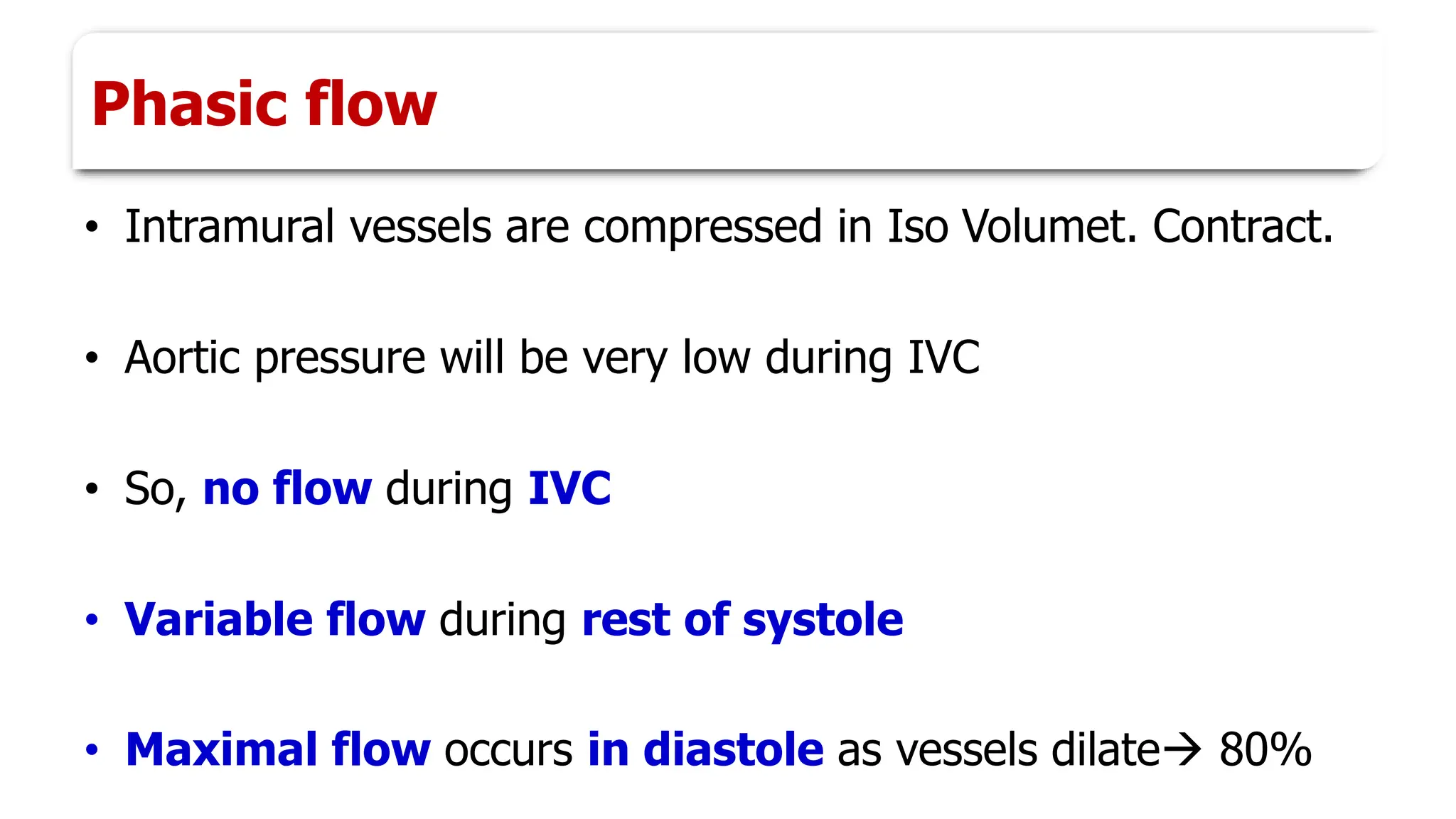
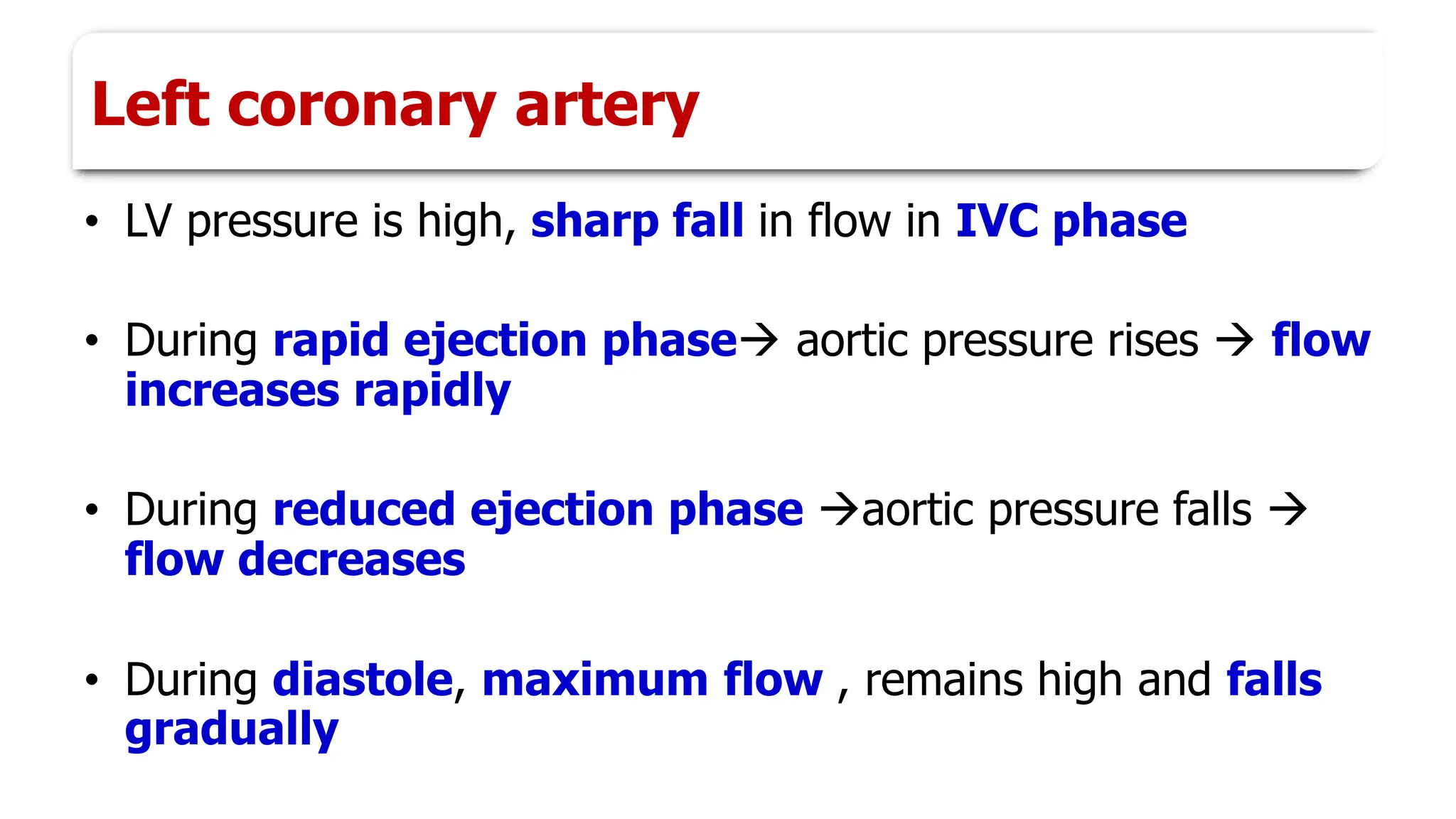
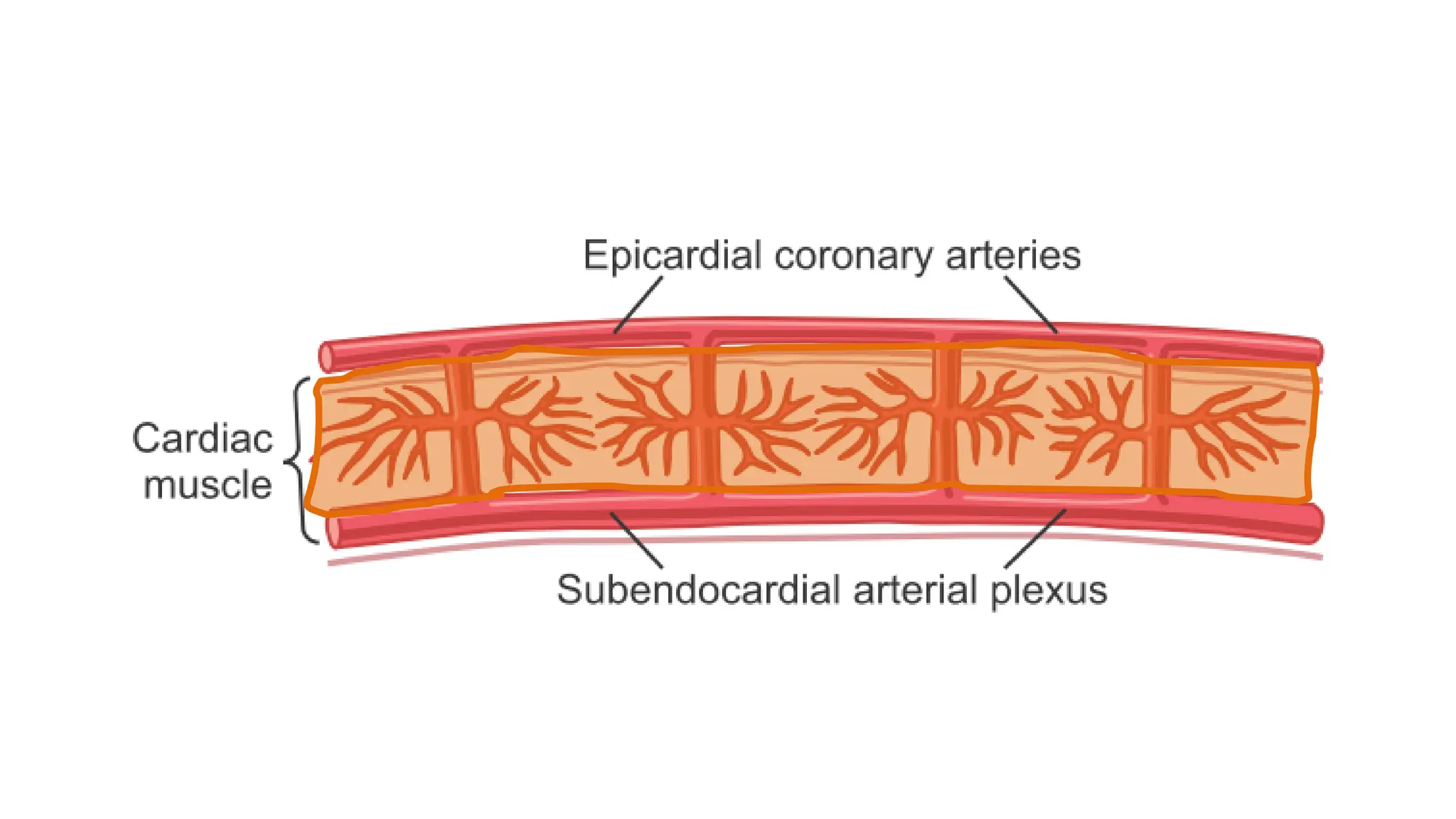
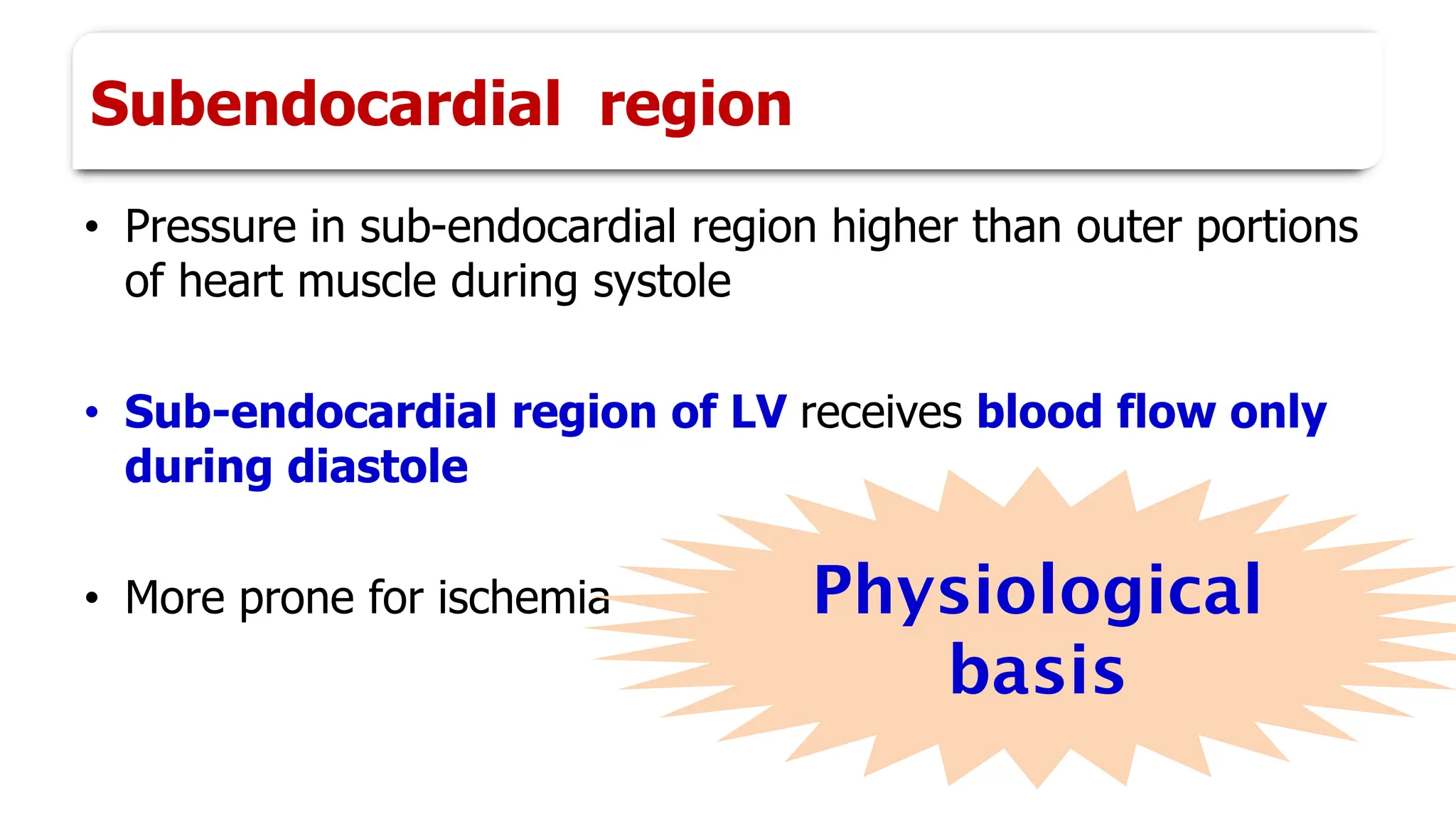
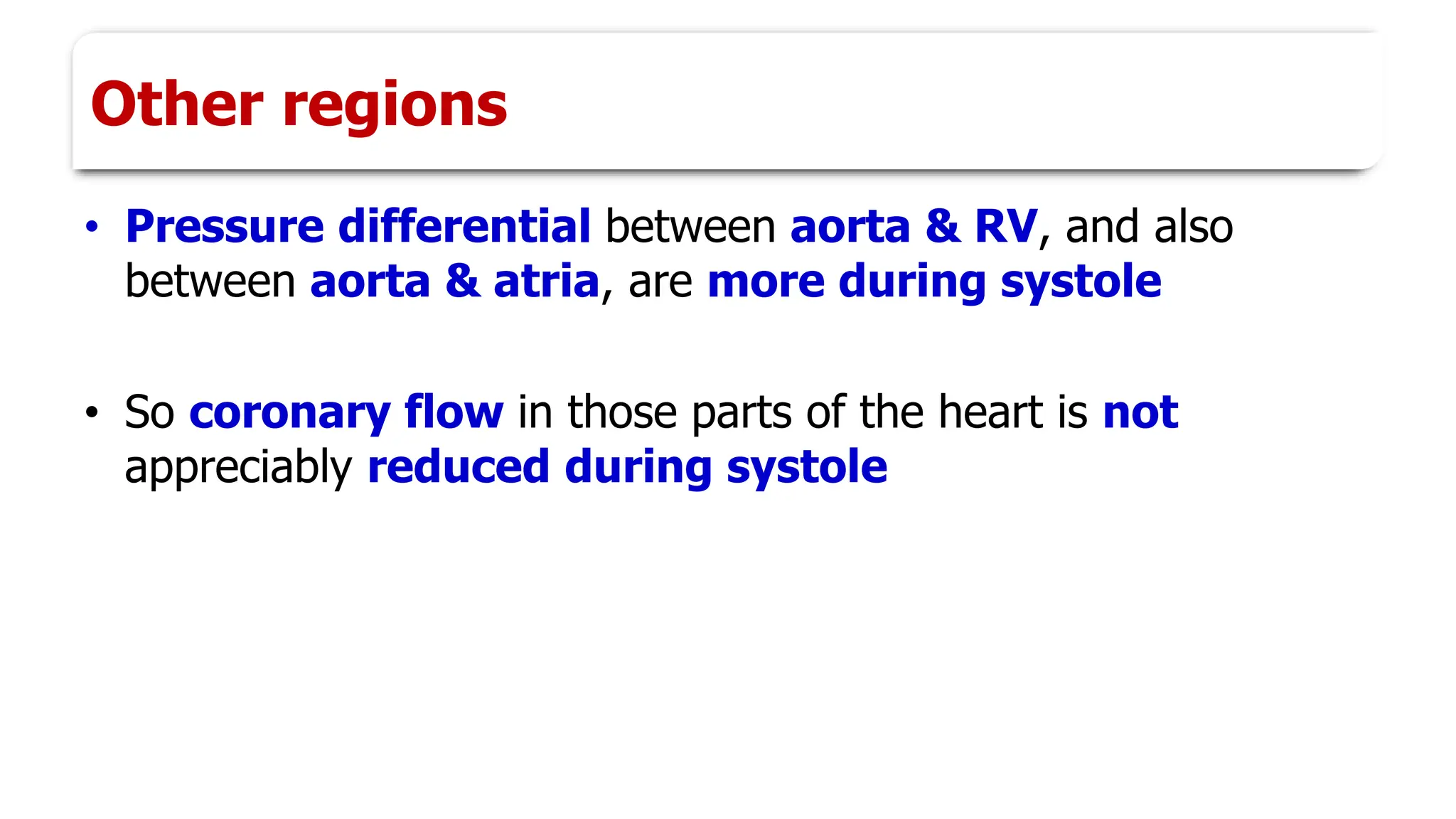
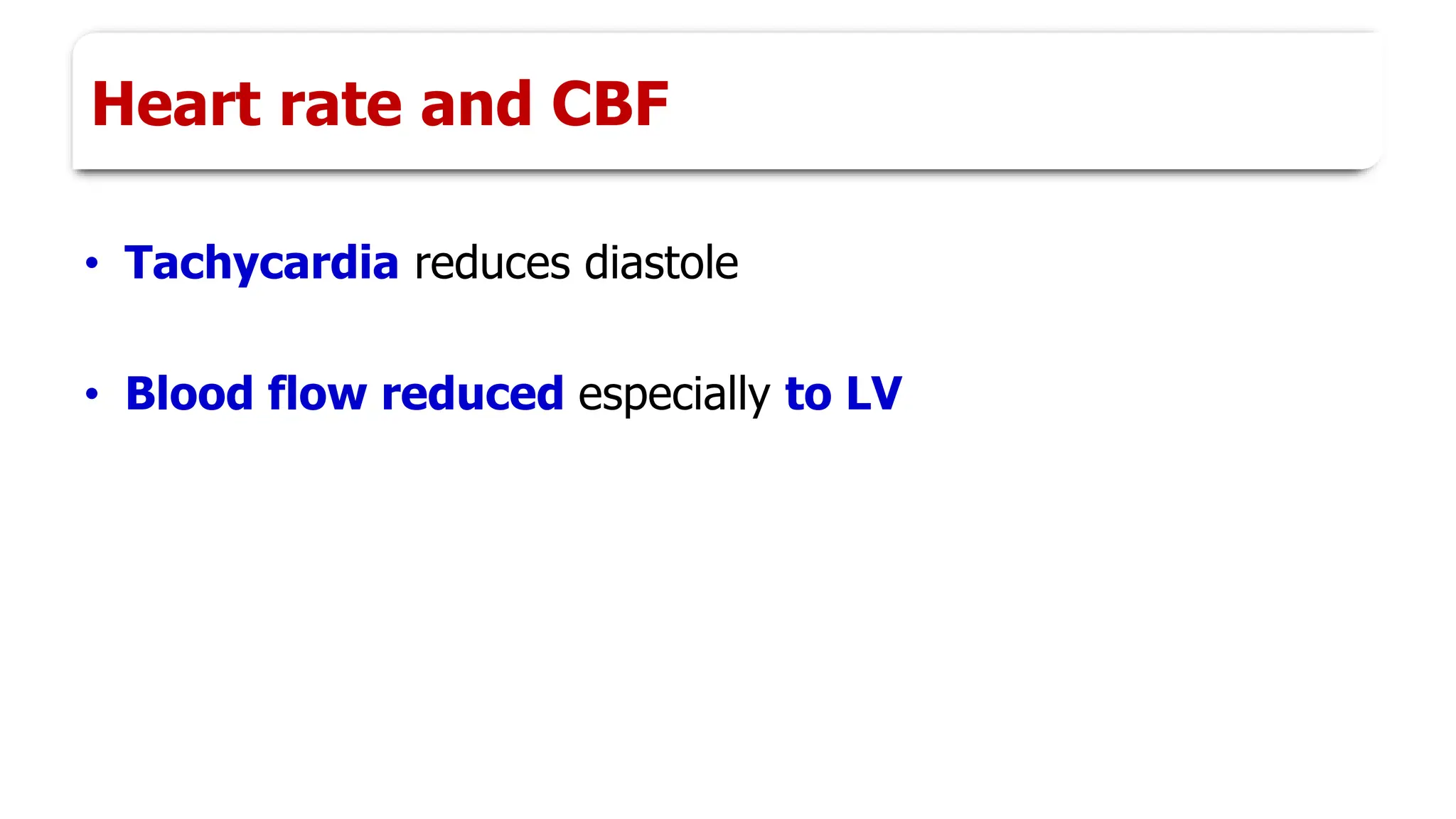
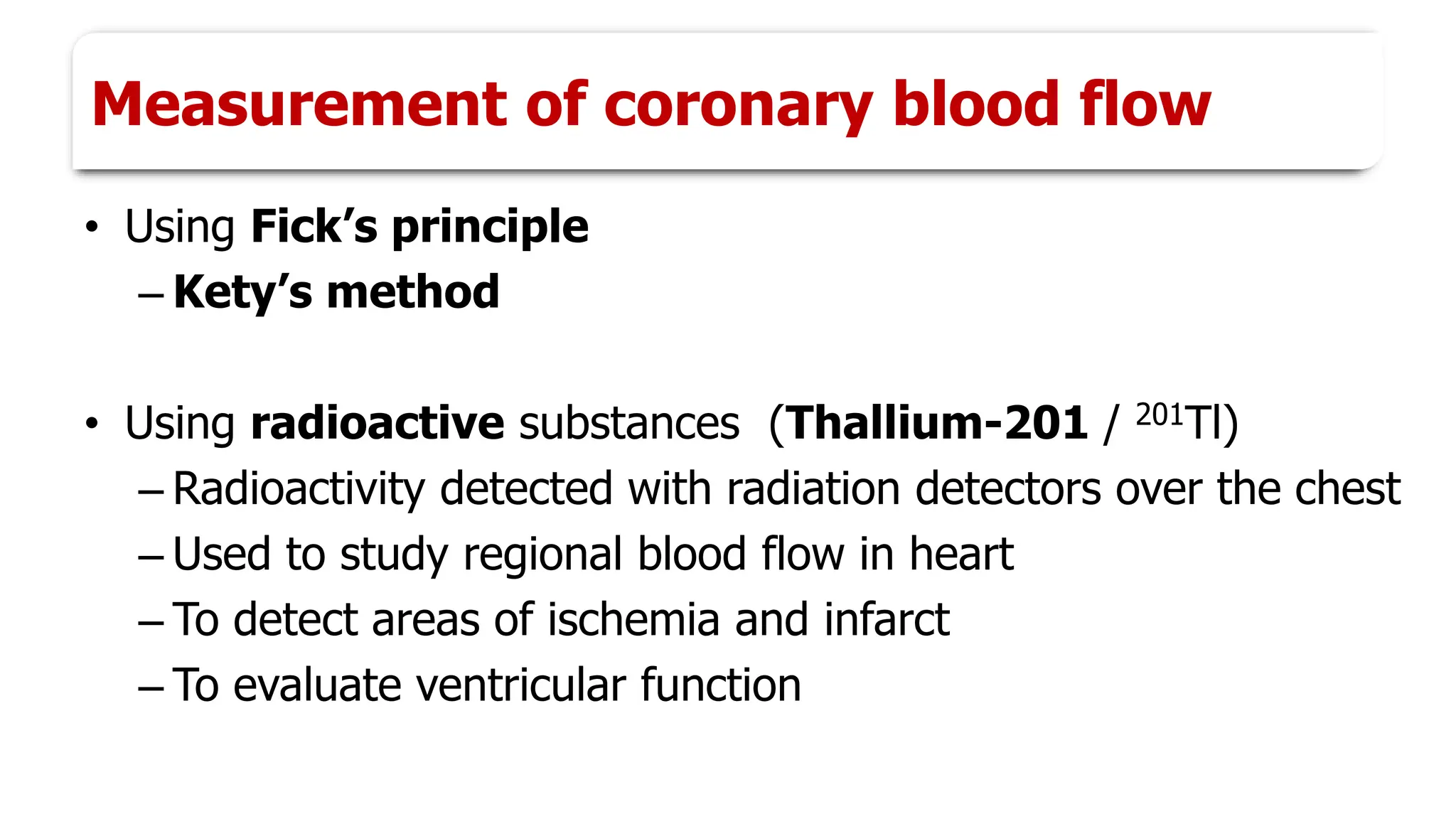
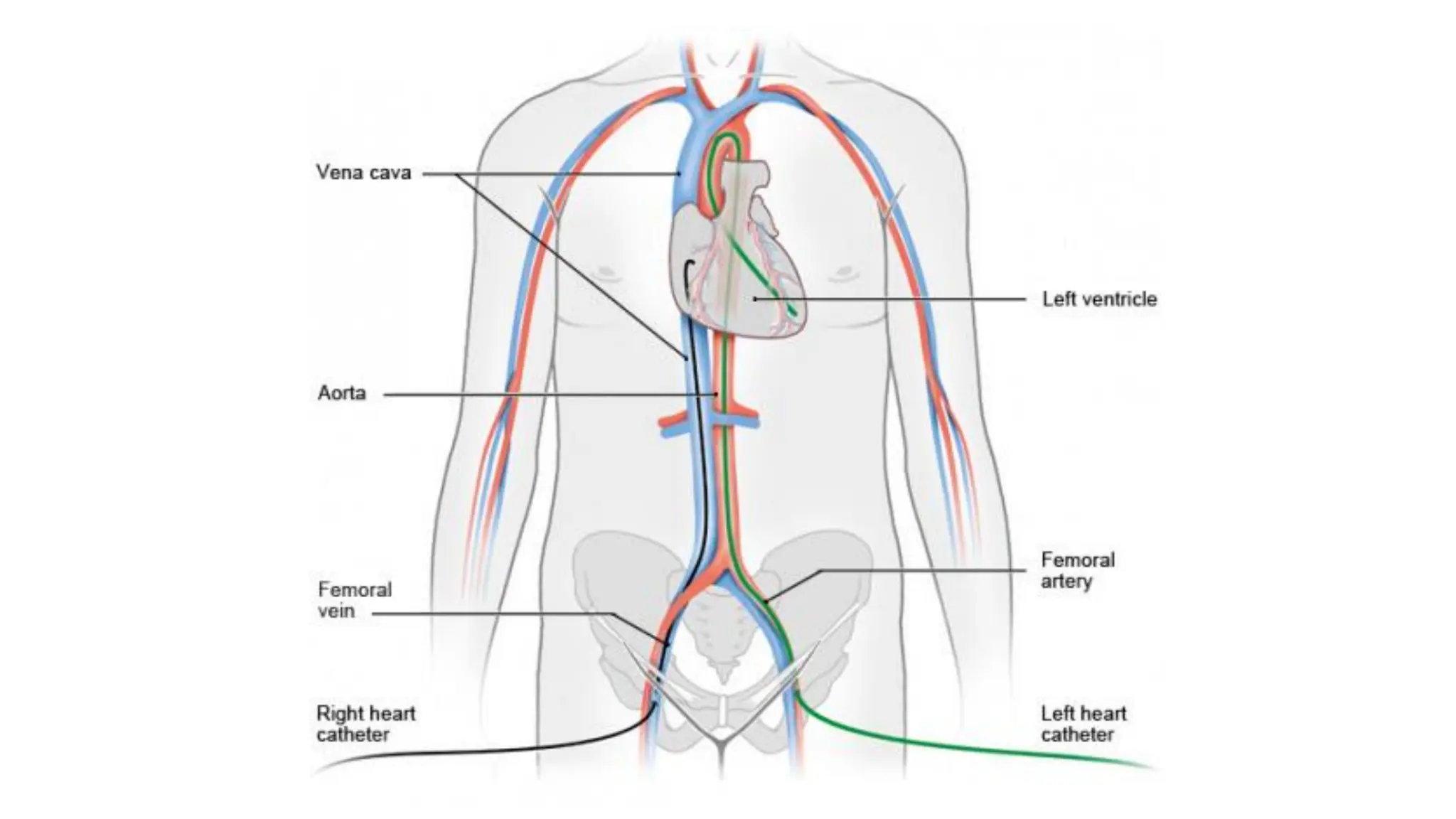
This document discusses coronary circulation. It will cover the functional anatomy of coronary blood flow, special features of coronary blood flow including phasic changes, measurement of coronary blood flow using techniques like Fick's principle, regulation of coronary blood flow through autoregulation and various chemical and neural factors, and insufficient coronary blood flow conditions like myocardial ischemia, angina pectoris, myocardial infarction, and their treatment and complications.