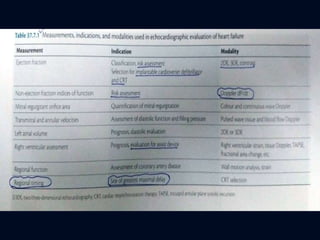
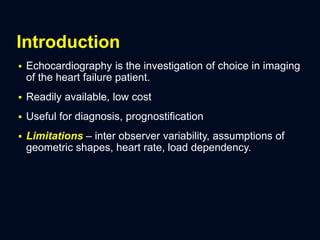
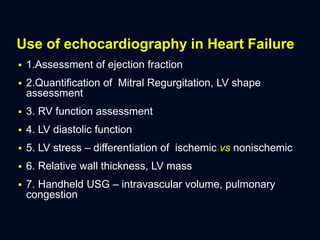
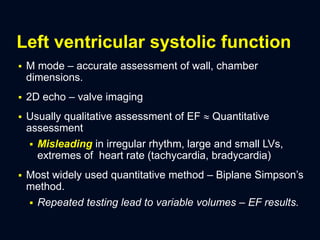
Echocardiography is a useful tool for diagnosing and monitoring heart failure patients. It can assess left ventricular ejection fraction, ventricular sizes and wall thickness, valve function, diastolic function, and pulmonary pressures. New techniques such as 3D echocardiography and strain imaging provide more accurate measurements of cardiac structure and function compared to older 2D techniques. Echocardiography is also used to differentiate the causes of heart failure, monitor for complications, and predict patient outcomes. It remains an important part of the evaluation and management of patients with heart failure.
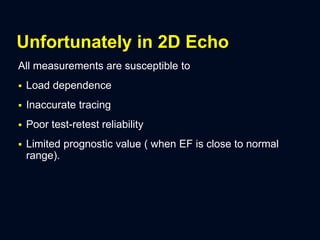
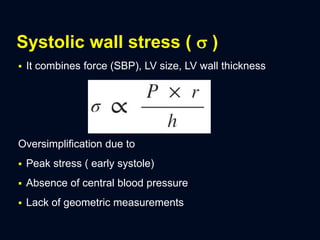
![ LVESWS= (0.334 P(LVID)/PWT [1 + PWT/LVID])
LVESWS – LV end systolic wall stress
LVID – Left ventricle inner diameter
PWT – posterior wall thickness
P – SBP](https://image.slidesharecdn.com/heartfailure-echocardiography-200409192521/85/Heart-failure-Echocardiography-12-320.jpg)