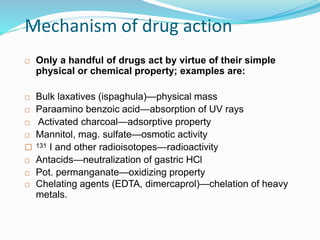
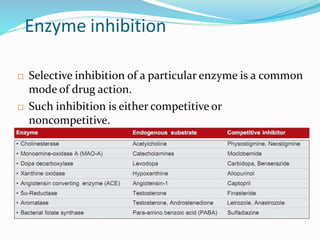
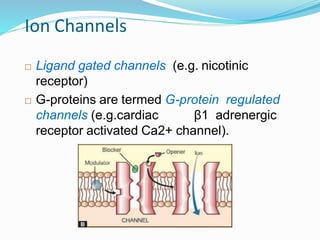
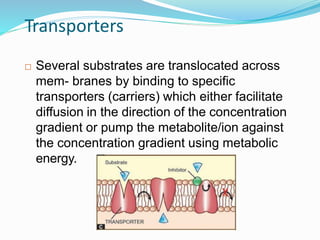
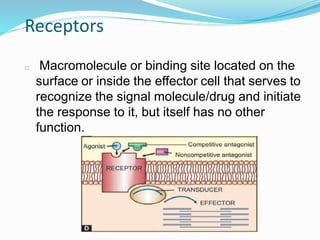
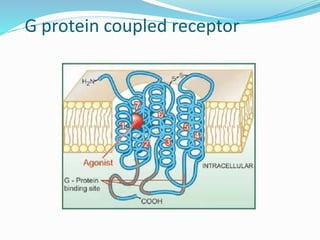
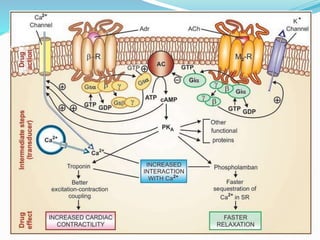
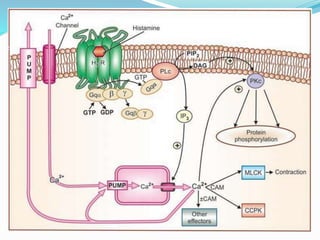
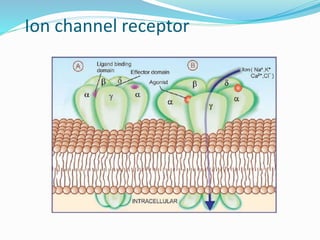
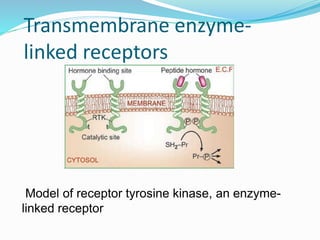
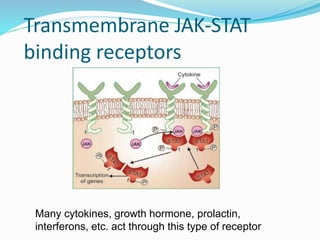
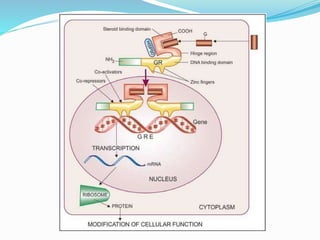
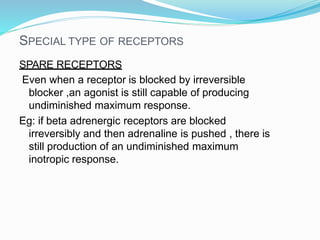
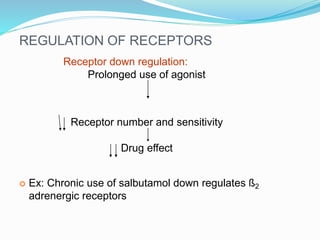
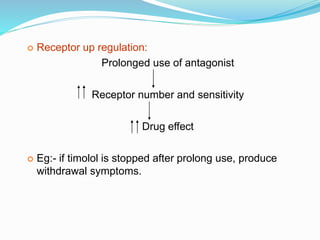
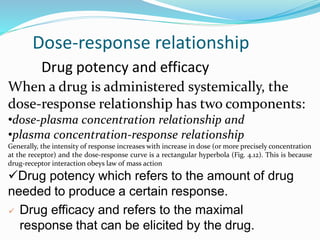
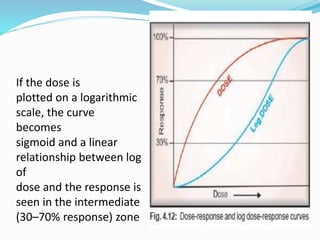
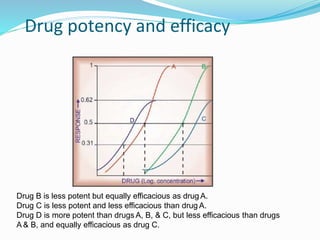
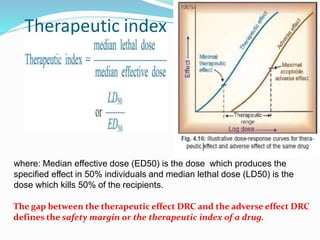
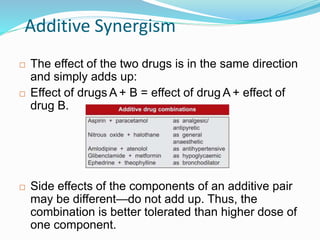
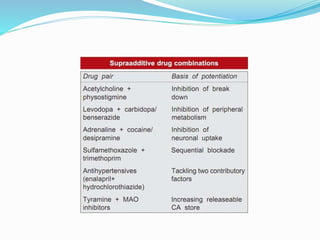
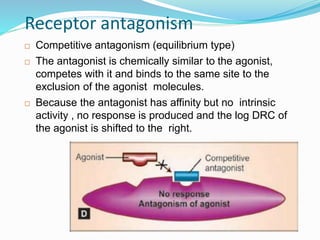
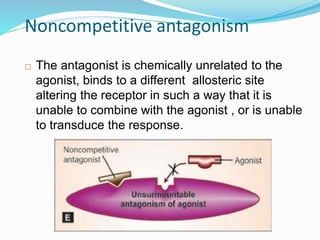
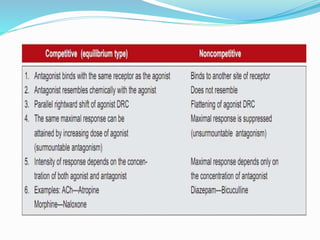
The document discusses the mechanisms of drug action, which can generally be categorized into four types: enzymes, ion channels, transporters, and receptors. It provides examples for each category and describes how drugs can interact with these biomolecules to produce their effects. For receptors specifically, it defines terms like agonist, antagonist, partial agonist, and discusses different receptor families like G-protein coupled receptors and enzyme-linked receptors. It also touches on concepts like drug potency, efficacy, therapeutic index, synergistic and antagonistic drug interactions.