1. Pharmacodynamics is the study of drug effects and how drugs produce their effects.
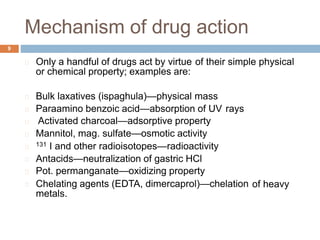
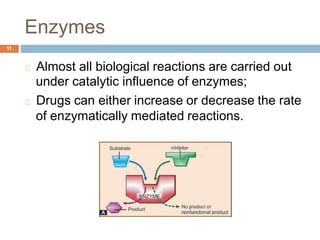
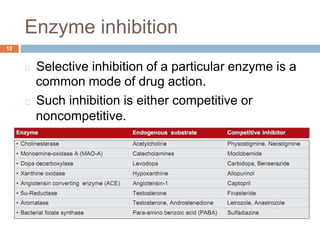
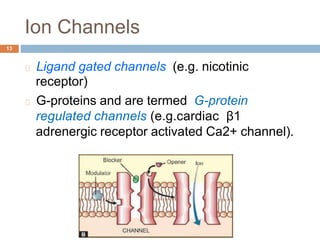
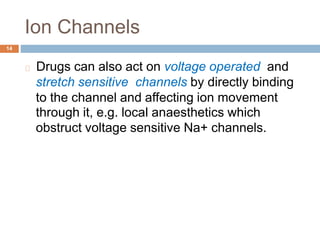
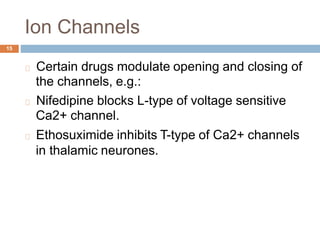
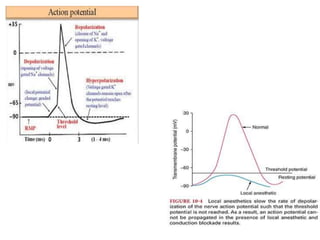
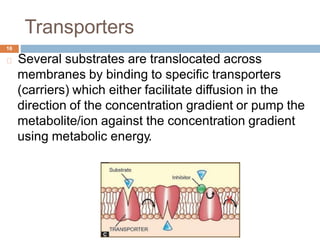
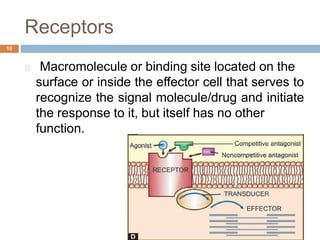
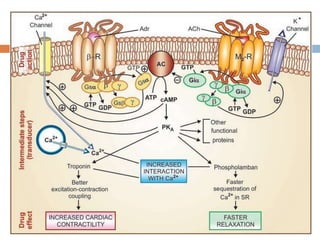
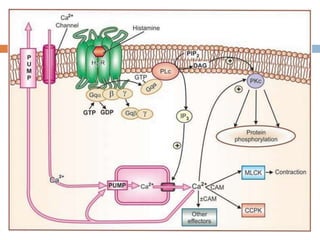
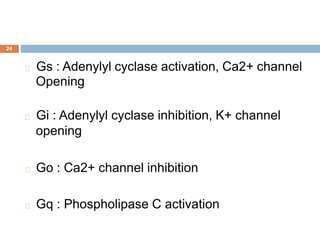
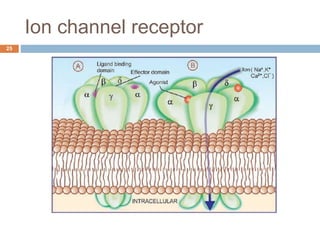
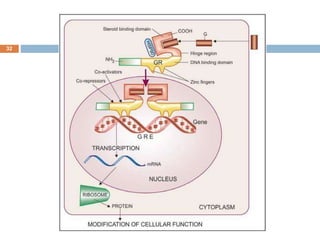
2. Drugs can produce effects through stimulation, depression, irritation, replacement, or cytotoxic action on cells. The majority of drugs interact with specific protein targets like enzymes, ion channels, transporters, and receptors.
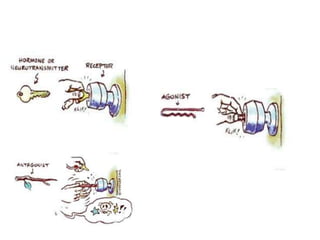
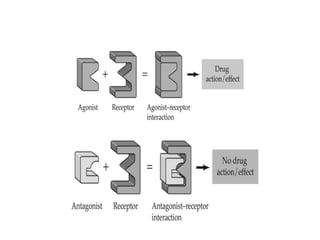
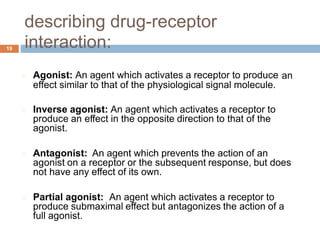
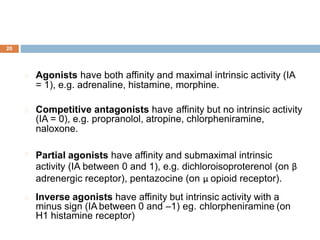
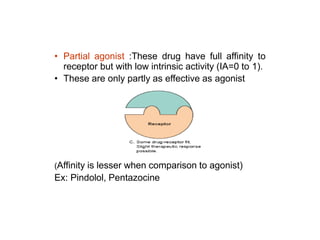
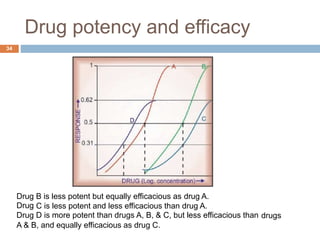
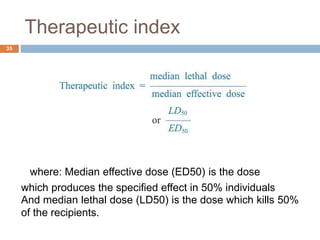
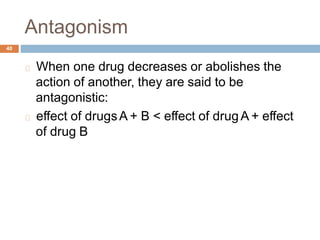
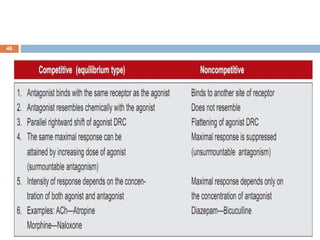
3. Drug interactions with targets can be agonistic, antagonistic, or otherwise modulate the target's function. Understanding a drug's potency, efficacy, therapeutic index, and interactions provides insight into its pharmacological effects.