This document provides information about Perthes disease, including:
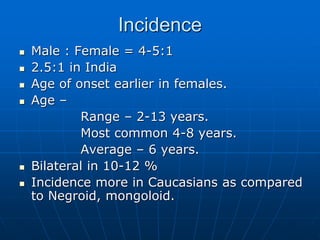
- It is a self-limiting condition caused by ischemia and necrosis of the femoral head, most common in children aged 4-8.
- Historical figures who studied the condition include Legg, Calve, and Perthes.
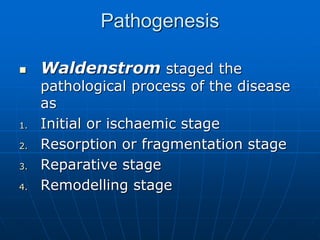
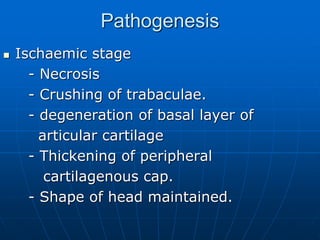
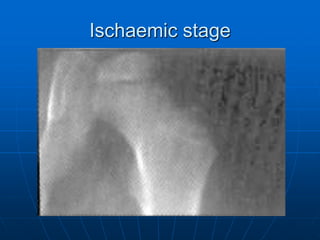
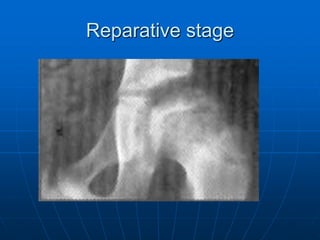
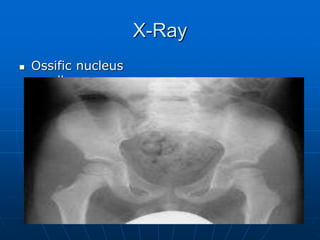
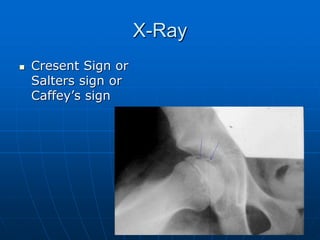
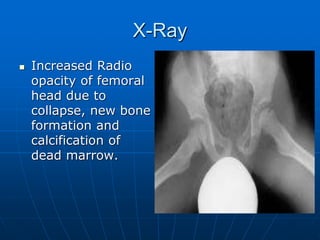
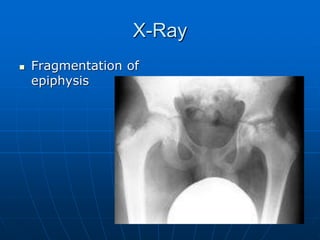
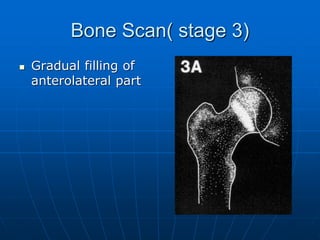
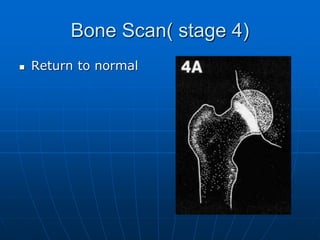
- The disease involves four stages: ischemic, fragmentation, reparative, and remodeling.
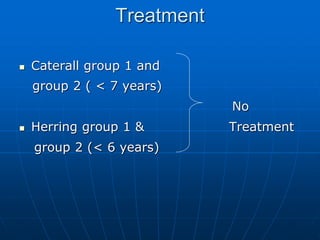
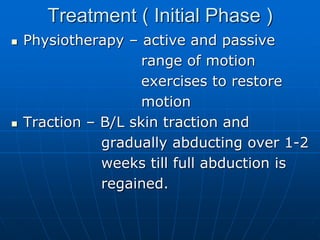
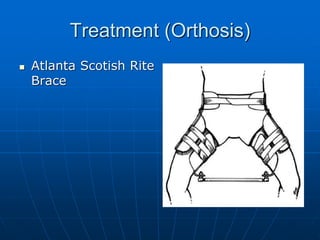
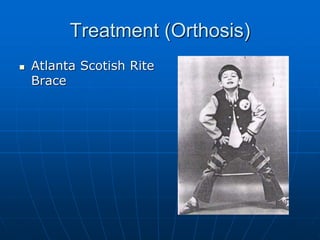
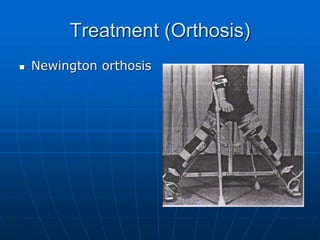
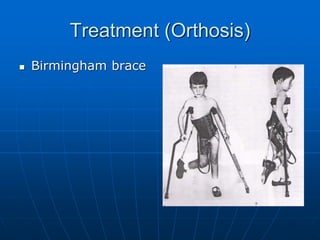
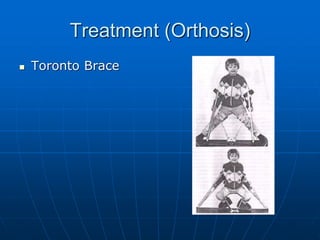
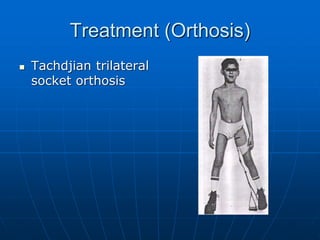
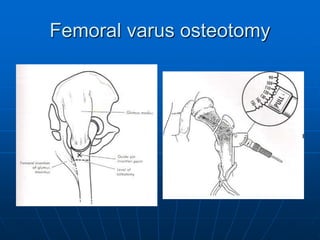
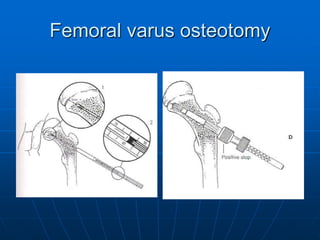
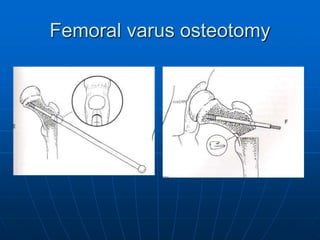
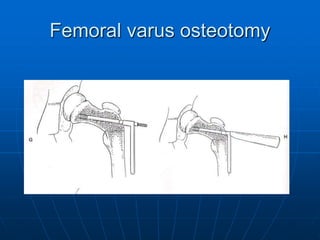
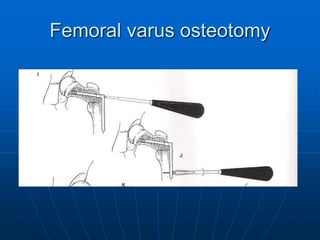
- Treatment aims to restore mobility, contain the femoral head, and allow weight bearing, through methods like bracing or osteotomies.
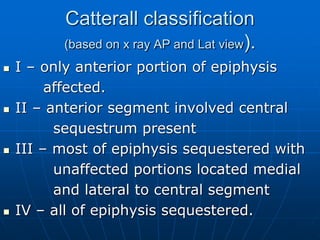
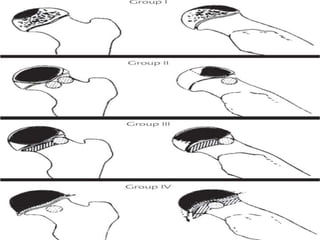
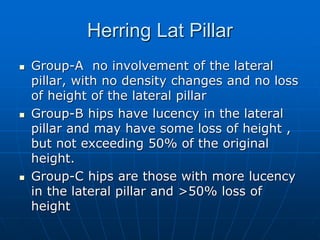
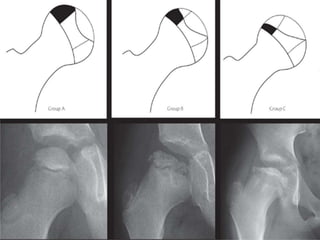
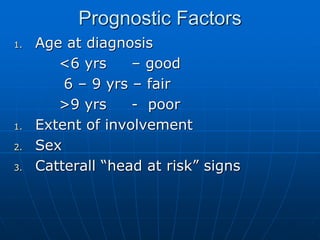
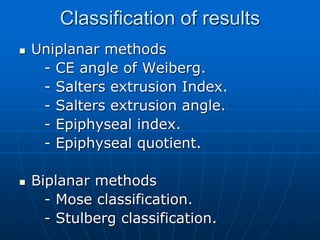
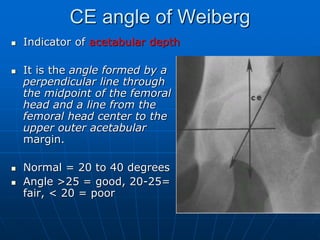
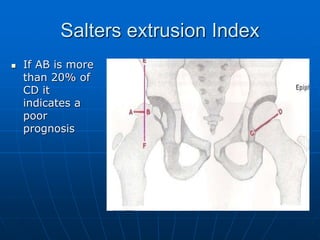
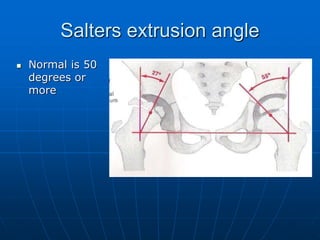
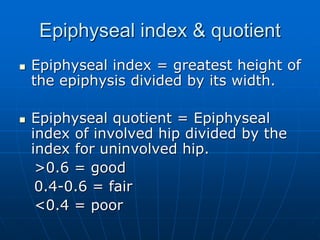
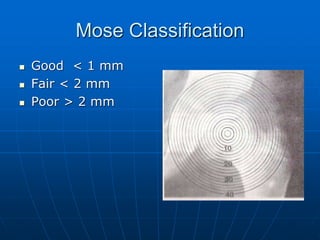
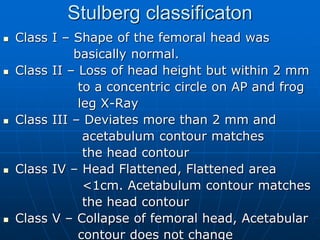
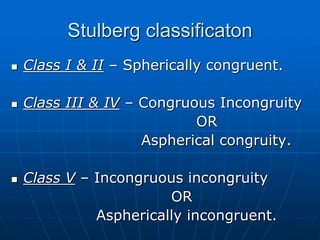
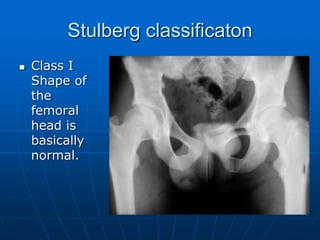
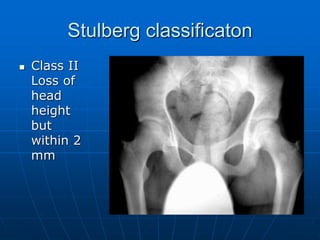
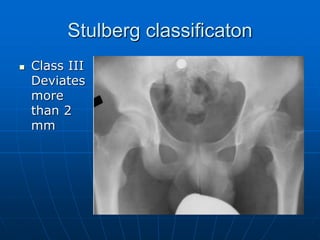
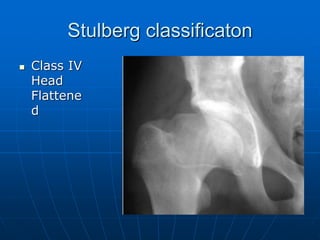
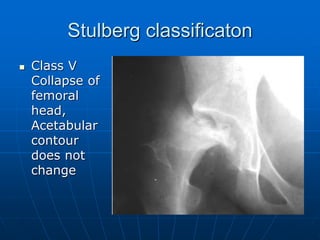
- Prognosis depends on factors like age of onset, extent of involvement, and classification system used to assess deformity and congruence.