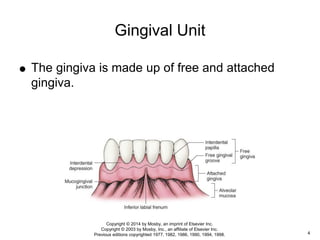
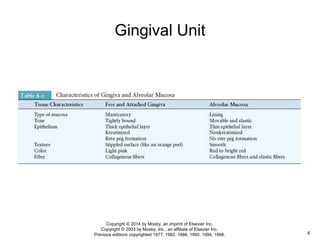
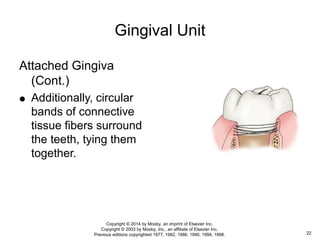
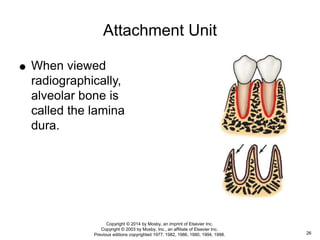
The periodontium consists of tissues that support the teeth and is divided into the gingival unit and attachment unit. The gingival unit includes the gingiva, free gingiva, attached gingiva, alveolar mucosa, and forms the visible part of the supporting structure. The attachment unit attaches the tooth to bone and includes the cementum, periodontal ligament, and alveolar bone. Together, the periodontium provides structural support to the teeth and also performs nutritive, sensory, and formative functions to maintain attachment.