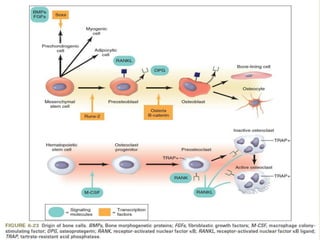
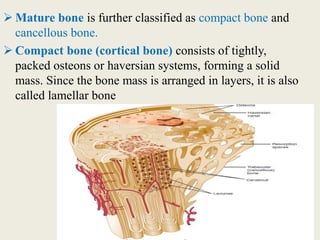
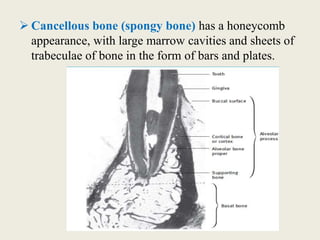
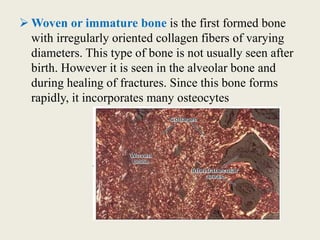
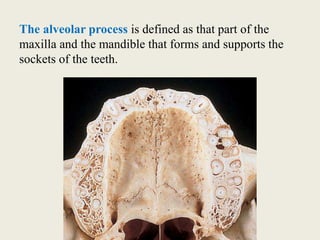
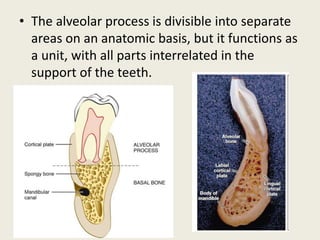
Bone is a living tissue that provides structure and support. It can be classified based on shape, development, histology, and composition. The alveolar process forms with tooth development and eruption to support teeth in the jaw. It consists of cortical and cancellous bone layers surrounded by osteoblasts and osteoclasts, which build and resorb bone through various signaling pathways and enzymes.
![COMPOSITION OF BONE
• Bone is a connective tissue composed of cells, fibers
and ground substance.
• The inorganic part of bone is made of bone minerals.
• The mineral component is composed of
hydroxyapatite crystals(Ca10[PO4]6[OH]2).
• Bone crystals are packed closely with long axis
nearly parallel to collagen fibrils axis.
• The ions present are calcium phosphate, hydroxyl and
carbonate. Citrate, magnesium, sodium, potassium,
fluoride, iron, zinc, copper, aluminum, lead,
strontium, silicon and boron are present in small
quantities.](https://image.slidesharecdn.com/presentation1-180724143137/85/ALVEOLAR-BONE-11-320.jpg)