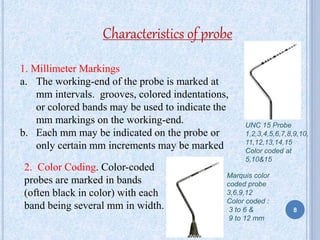
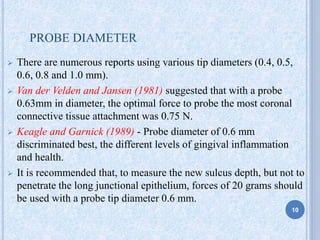
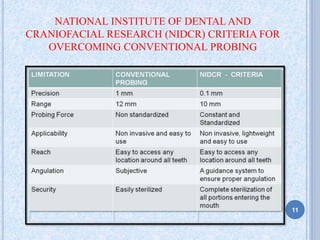
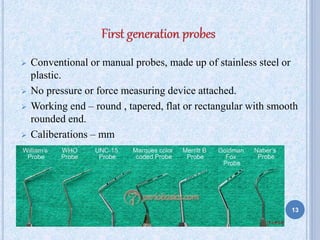
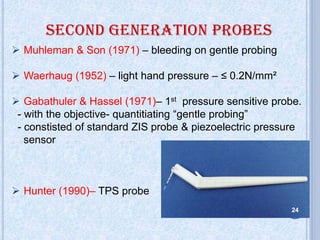
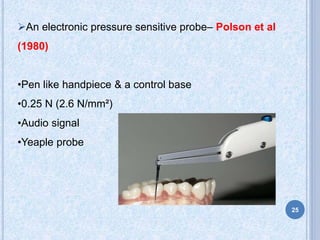
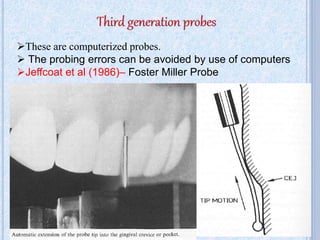
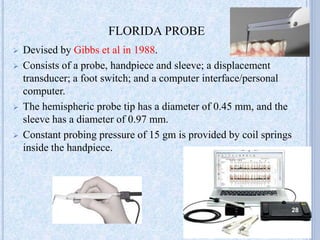
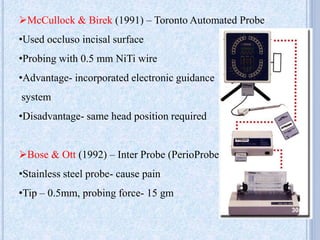
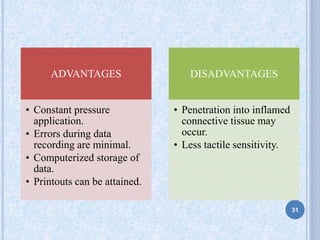
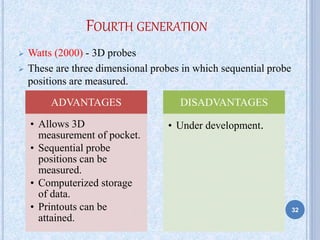
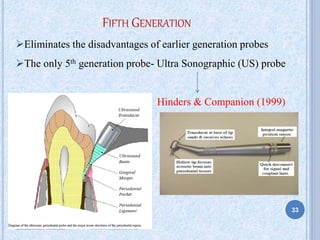
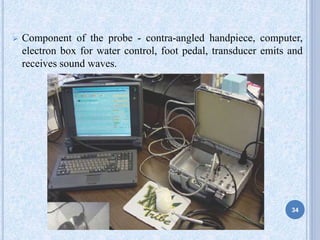
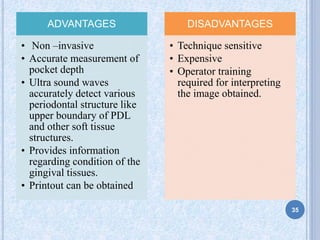
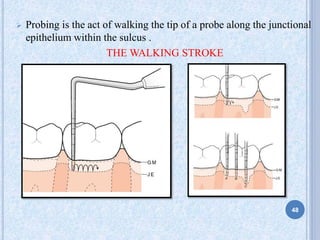
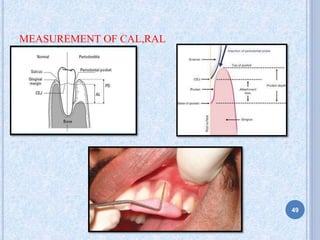
This document provides an overview of periodontal probes, including their history, uses, classifications, and related studies. Periodontal probes are calibrated instruments used to measure pocket depth and determine pocket configuration. Several generations of probes have been developed over time, with modifications including standardized tip diameters and shapes, millimeter markings, and the incorporation of pressure sensors. Current probes range from conventional manual probes to computerized probes that can precisely measure probing force and position. Probes are a key diagnostic tool in periodontal examinations and assessments of treatment outcomes.