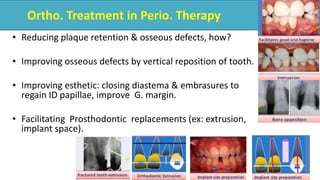
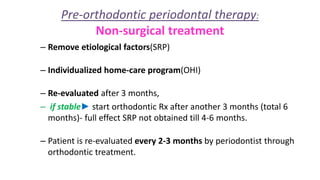
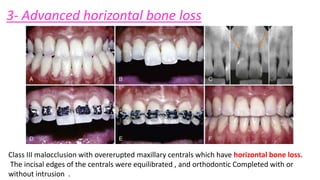
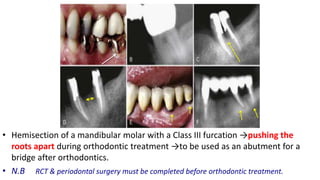
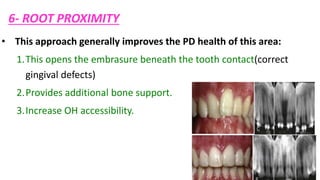
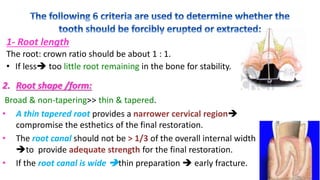
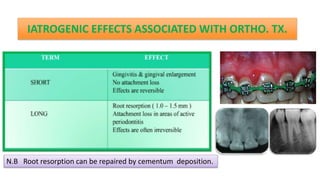
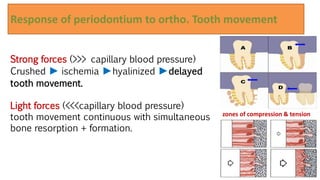
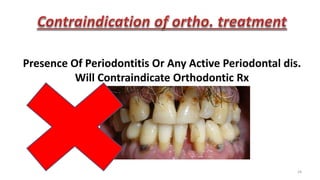
The document discusses the integration of orthodontic treatment with periodontal therapy, emphasizing the importance of managing osseous defects and improving esthetics before beginning orthodontic procedures. It outlines various types of periodontal issues and their corresponding treatments, including surgical and non-surgical approaches, to ensure patient stability prior to orthodontics. Additionally, it details the considerations for implants, tooth erosions, and gingival discrepancies associated with orthodontic movements.