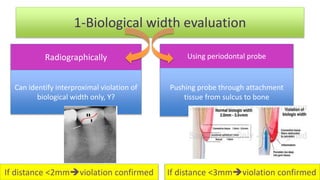
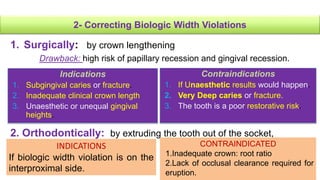
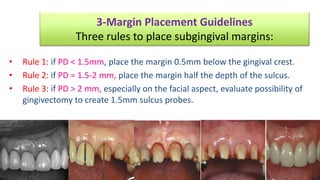
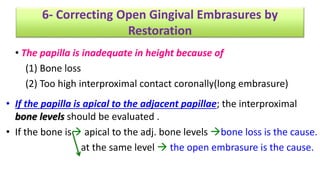
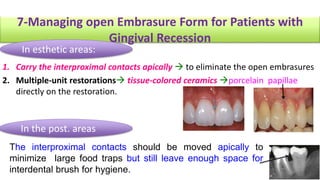
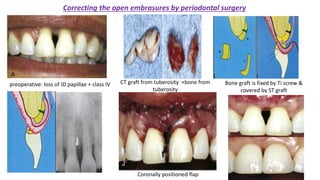
The document discusses the preparation of the periodontium for restorative dentistry, emphasizing the importance of treating active periodontal infection and maintaining healthy periodontium for successful treatments. It outlines a sequenced approach involving periodontal surgeries, management of mucogingival problems, and guidelines for margin placements in restorative procedures to ensure proper aesthetics and function. Key considerations include controlling periodontal inflammation, evaluating biological width, and correcting open gingival embrasures to enhance restorative outcomes.